We couldn't live without acetylcholine (ACh). It's an important neurotransmitter within the body and, in fact, was the very first neurotransmitter discovered. The moving title of this article was chosen to impress upon the reader the importance of this neurotransmitter to processes within the body that require movement, from skeletal muscle or smooth muscle. It's also vitally important for brain function, playing a key role in memory, learning and cognition. It functions to relay signals from one neuron to another in the central nervous system and from a neuron to a muscle fiber in the peripheral nervous system. The production of ACh, symptoms and causes of deficiency and how best to treat low ACh will be discussed, but first we'll start with a basic physiology lesson to help you appreciate the function of ACh within the nervous system.
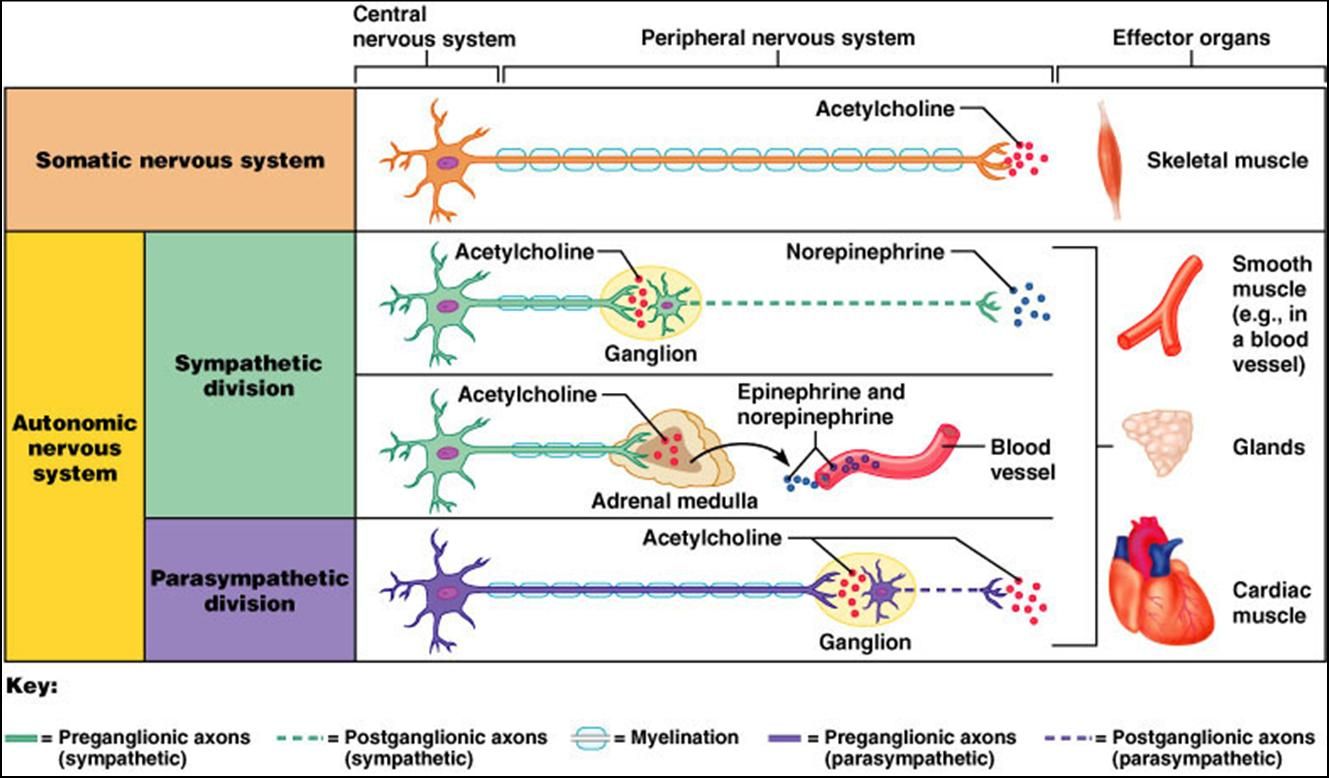
The nervous system is divided into two branches called the autonomic and somatic nervous systems. The autonomic nervous system is our "automatic" nervous system that we cannot voluntarily control. If you get sweaty when nervous or your heart rate increases when you're excited that's your autonomic nervous system controlling your body's response. Your somatic nervous system is your "voluntary" nervous system. This part of the nervous system controls skeletal muscles, like those in my fingers as I type this. You can see from image 1 that ACh is used in both of these branches of the nervous system.
The autonomic nervous system is further divided into the sympathetic and parasympathetic branches of the nervous system. The parasympathetic nervous system is engaged most of the time in a healthy person. The sympathetic nervous system becomes engaged during times of stress or excitement. The sympathetic branch uses ACh to relay messages but also uses epinephrine and norepinephrine. The parasympathetic nervous system relies solely on ACh to function properly. The parasympathetic nervous system is important for proper digestion, gut motility, salivary flow, lacrimation (tears) and bladder function. The nerve fibers of the parasympathetic nervous system originate from the brain stem and sacral region. The parasympathetic nerve fibers originating from the brain stem are cranial nerves III, VII and IX. Cranial nerve X, the vagus nerve, also contains parasympathetic nerve fibers. A well-functioning vagus nerve is extremely important for all aspects of digestion including stomach acid secretion, pancreatic secretion, bile flow and peristalsis, which is the wave of muscle that moves food through the intestines. (Stakenborg, 2013) The vagus nerve is also very important for regulating heart rate. ACh creates an inhibitory response to cardiac muscle resulting in a slowed heart rate. This is different than other receptors within the parasympathetic system that result in a general increase in activity.
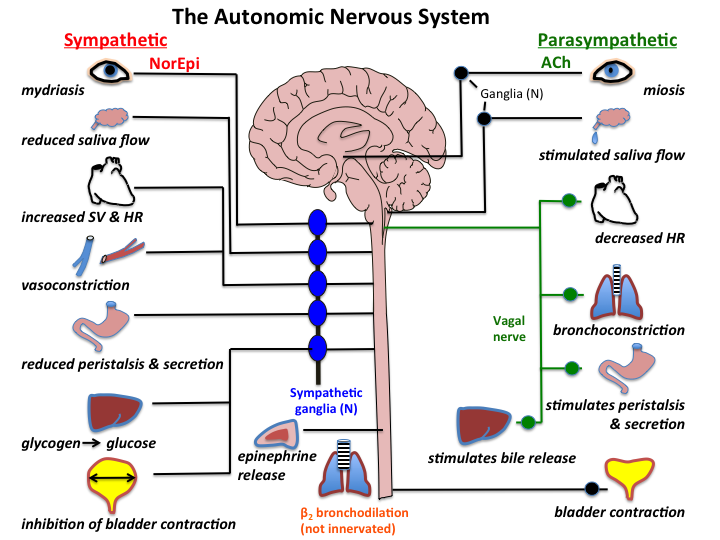
By reviewing the different functions of the sympathetic and parasympathetic nervous system in image 2 one can already start to get an idea of what a deficiency in ACh might look like. The symptoms of deficiency are as follows:
Symptoms of Acetylcholine Deficiency
- Constipation/gastroparesis
- Memory problems
- Difficulty with word recall when speaking
- Learning difficulties
- Dry mouth
- Dry eyes
- Orthostatic hypotension
- Low muscle tone
- Depressed mood
- Fast heart rate
- Chronic inflammation
- Emotional instability
Because ACh is so important for nervous system conduction within the brain, a deficiency in ACh has been linked to Alzheimer's disease (AD) and dementia. (Francis, 2005) The enzyme that breaks down acetylcholine is called acetylcholinesterase. Several drugs have been developed for the treatment of Alzheimer's disease that inhibit this enzyme thus increasing ACh levels. These drugs are donepazil, rivastigmie, galantamine. These drugs have not been shown to reverse the effects of AD, they merely stabilize or slow the rate of cognitive decline. As well, some patients don't respond at all to them. (O'Brien, 2010) They also have many side effects due to their systemic effects of increasing ACh levels throughout the body when the goal is to increase ACh in the brain alone. Some of the side effects include nausea, vomiting, diarrhea, muscle cramps, weight loss, headache, insomnia, hallucinations, fatigue, hypertension and frequent urination. (medicine.net)
It's possible that the decline in acetylcholine levels in AD and dementia are due to a deficiency in the precursors needed to make it. So, let's talk about how acetylcholine is made next.
It's possible that the decline in acetylcholine levels in AD and dementia are due to a deficiency in the precursors needed to make it. So, let's talk about how acetylcholine is made next.
Acetylcholine synthesis
The synthesis of acetylcholine is actually fairly simple as a whole, yet complex in the details. To make acetylcholine we need choline and an acetyl group. The preferred source for the acetyl group is acetyl CoA which is derived from pyruvate, the end product of glycolysis. Research showing this dates as far back as 1936 when scientists incubated animal brain cells in various medium and found that glucose, pryuvate and lactate all equally resulted in an increase in ACh production. Oxygen was needed as well. They stated, "We know now, of course, that acetylCoA (AcCoA) is required for ACh biosynthesis and that it must be the substance produced during the combustion of glucose, lactate or pyruvate in the brain that gives rise to ACh." (Quastel, 1936) Their work was corroborated by researchers in 1979 who stated, "Acetylcholine is synthesized from acetyl CoA and choline in the cytoplasm. Glucose and pyruvate are the preferred precursors of the acetyl carbons of acetylcholine in adult mammalian brain." (Gibson, 1979)
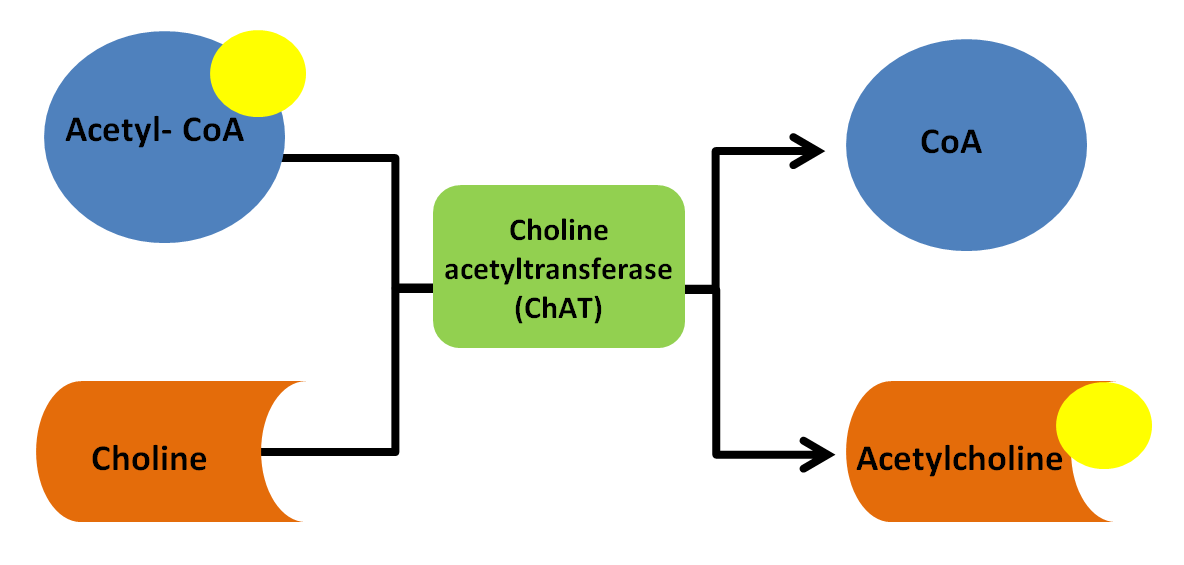
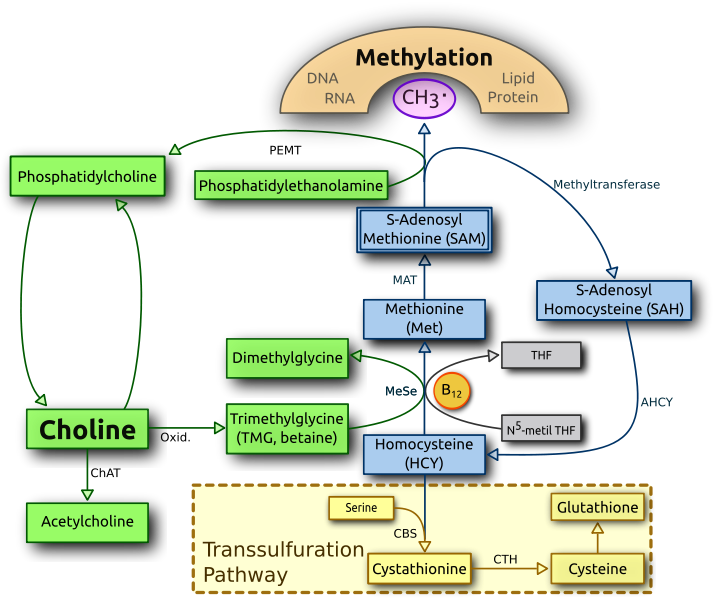
The enzyme that cleaves the acetyl group from acetyl CoA and attaches it to choline is choline acetyltransferase (ChAT) as seen in image 3.
The enzyme that cleaves the acetyl group from acetyl CoA and attaches it to choline is choline acetyltransferase (ChAT) as seen in image 3.
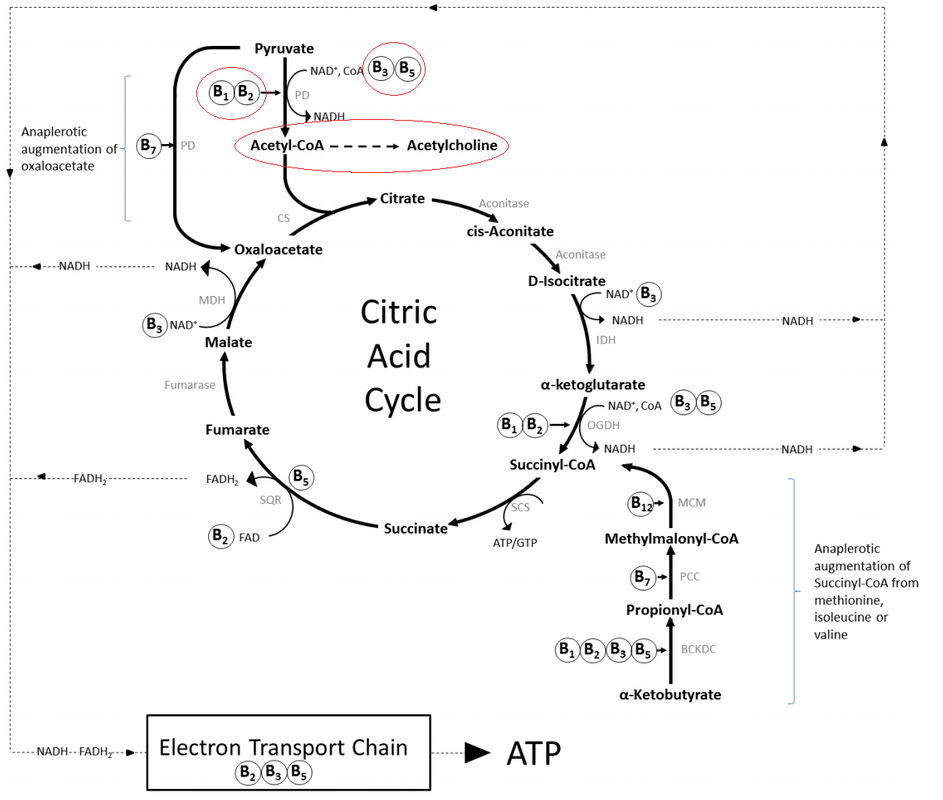
So, how do we then get acetyl CoA from glucose and pyruvate? This is where it gets a little more complicated. Those who have studied and understand the Citric Acid Cycle will recognize this information. For those who haven't studied this: the Citric Acid Cycle is a key process involving many steps by which mitochondria make energy. This process is heavily dependent on B vitamins. Image 4 shows the many steps and enzymes involved in this process along with the B vitamins that act as cofactors for those enzymes. The one enzyme I will focus on here is PD that is seen below pyruvate at the top of image 4. PD stands for pyruvate dehydrogenase. It's role is to convert pyruvate into acetyl-CoA.
(Image Source: B Vitamins and the Brain: Mechanisms, Dose and Efficacy—A Review)
I've discussed pyruvate dehydrogenase before in my lecture "Thiamine Deficiency in Children with Special Needs". I've posted the whole lecture below for those who want to know all of the details.
Essentially PD is dependent on adequate levels of thiamine (B1), riboflavin (B2), alpha lipoic acid and niacinamide (B3). In addition, the precursor to coenzyme A (CoA) is pantothenic acid (B5). All of these B vitamins must be present in adequate amounts in order for acetyl CoA to be made. (Stacpoole, 2012) Particularly noteworthy is the role that thiamine plays in ACh production. "The role of thiamine as a crucial coenzyme in neuronal metabolism of carbohydrates and neurotransmitters, especially acetylcholine, has been well elucidated." (Hirsch, 2011) The administration of benfotiamine, a form of thiamine, alone has been shown to reverse the symptoms of Alzheimer's disease, which has been linked to low ACh levels. (Pan, 2016)
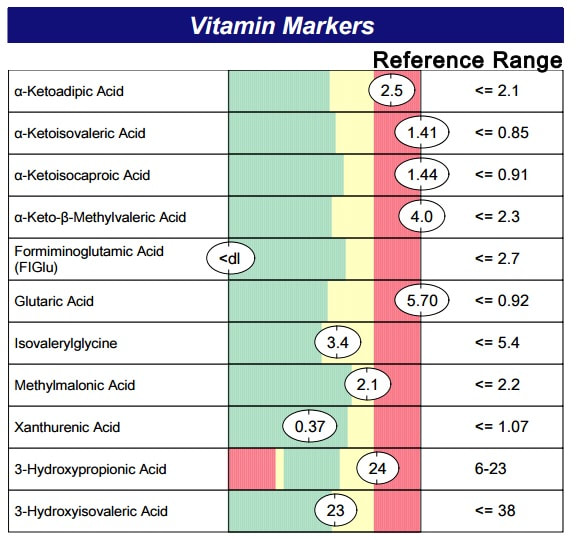
Deficiencies in these B vitamin cofactors is most often due to gastrointestinal malabsorption. Yeast overgrowth is a common cause of malabsorpton, especially of B vitamins. The best testing to determine a need for these B vitamins is organic acid testing. Results like the ones seen in image 5, for example, indicate a significant deficiency in B1, B2, B3 and B5. These are results for a child who has Down syndrome and is likely also deficient in ACh due to her B vitamin deficiencies, not her extra chromosome. The deficiencies in this child were due to small intestinal bacterial and fungal/candida overgrowth. Addressing these deficiencies along with the root cause of malabsorption is key to optimizing ACh synthesis.
Deficiencies in these B vitamin cofactors is most often due to gastrointestinal malabsorption. Yeast overgrowth is a common cause of malabsorpton, especially of B vitamins. The best testing to determine a need for these B vitamins is organic acid testing. Results like the ones seen in image 5, for example, indicate a significant deficiency in B1, B2, B3 and B5. These are results for a child who has Down syndrome and is likely also deficient in ACh due to her B vitamin deficiencies, not her extra chromosome. The deficiencies in this child were due to small intestinal bacterial and fungal/candida overgrowth. Addressing these deficiencies along with the root cause of malabsorption is key to optimizing ACh synthesis.
That leaves us to discuss choline as the other important half of acetylcholine. Choline is an essential nutrient that must be obtained from the diet. Because it is water-soluble the body does not store it, so daily consumption of this nutrient is important for consistent production of acetylcholine to occur. Some choline synthesis within the body is possible, however the production of choline is heavily dependent on a properly functioning methylation cycle. Many genetic and environmental variables exist around methylation.
Foods highest in choline include eggs (yolks) and meat, so vegans and vegetarians are at risk for being low in choline. Supplementation is possible by taking lecithin sourced from soy or sunflower. Lecithin is rich in phosphatidylcholine (PC), which is a precursor to choline. Citicoline and CDP-choline are other forms of choline that have been shown to enhance memory and cogntion. (Gareri, 2015; Fioravanti, 2006) Choline bitartrate should be avoided. It's the most commonly used form because it's the cheapest. It also is the least reliable form for impacting brain levels of choline (Lippelt, 2016) I prefer PC over other sources of choline because the production of PC is the second largest draw on methylation than all other process that require methylation combined. (Bertolo, 2013) Image 5 shows the production of PC from phosphatidylethanolamine via PEMT (phosphatidylethanolamine N-methyltransferase), a process that occurs in the liver. Because cell membranes consist largely of PC the body is required to make it often to keep up with cellular repair and growth. By supplying PC as a supplement this eases up on methylation and allows more methyl groups to be used for other methylation dependent processes.
As well, supplementing with PC has been shown to increase acetylcholine synthesis. Dr. Steven Heizel from the Department of Nutrition, School of Public Health and School of Medicine at the University of North Carolina stated, "Acetylcholine synthesis can be influenced by the availability of choline...its manipulation by changing the diet is likely to be a powerful tool for improving human performance.". (Heizel, 2006)
Foods highest in choline include eggs (yolks) and meat, so vegans and vegetarians are at risk for being low in choline. Supplementation is possible by taking lecithin sourced from soy or sunflower. Lecithin is rich in phosphatidylcholine (PC), which is a precursor to choline. Citicoline and CDP-choline are other forms of choline that have been shown to enhance memory and cogntion. (Gareri, 2015; Fioravanti, 2006) Choline bitartrate should be avoided. It's the most commonly used form because it's the cheapest. It also is the least reliable form for impacting brain levels of choline (Lippelt, 2016) I prefer PC over other sources of choline because the production of PC is the second largest draw on methylation than all other process that require methylation combined. (Bertolo, 2013) Image 5 shows the production of PC from phosphatidylethanolamine via PEMT (phosphatidylethanolamine N-methyltransferase), a process that occurs in the liver. Because cell membranes consist largely of PC the body is required to make it often to keep up with cellular repair and growth. By supplying PC as a supplement this eases up on methylation and allows more methyl groups to be used for other methylation dependent processes.
As well, supplementing with PC has been shown to increase acetylcholine synthesis. Dr. Steven Heizel from the Department of Nutrition, School of Public Health and School of Medicine at the University of North Carolina stated, "Acetylcholine synthesis can be influenced by the availability of choline...its manipulation by changing the diet is likely to be a powerful tool for improving human performance.". (Heizel, 2006)
The stage of life that has been shown to be most dependent on dietary choline is fetal development. Dr. Heizel has written, "Choline is critical during fetal development, when it influences stem cell proliferation and apoptosis, thereby altering brain structure and function." (Heizel, 2006) Researchers recently tested two groups of mothers who were in their third trimester of pregnancy. They supplemented one group with 480 mg of choline per day and the second group received 980 mg of choline per day. They then followed up by testing the infants at 4, 7, 10 and 13 months old for processing speed and visuospatial memory. Their results showed "maternal consumption of approximately twice the recommended amount of choline during the last trimester improves infant information processing speed." (Canfield, 2018)
Genetic variations in mothers can alter choline requirements as well. Specifically variations in PEMT and MTHFR1 genes can alter endogenous synthesis of choline. Maternal dietary choline intake can influence global gene methylation and ultimately gene expression in the unborn child. (Bennett, 2016). Because not all mothers know their PEMT or MTHFR1 gene status supplementing with choline during pregnancy at approximately 980 mg per day, as was done in the study above, may help to ensure adequate levels are available for proper infant brain development. In addition, vegans are at high risk for being choline deficient and should definitely consider supplementing. Vegetarians who eat eggs daily are less likely to be deficient. One egg contains about 150 mg of choline.
Genetic variations in mothers can alter choline requirements as well. Specifically variations in PEMT and MTHFR1 genes can alter endogenous synthesis of choline. Maternal dietary choline intake can influence global gene methylation and ultimately gene expression in the unborn child. (Bennett, 2016). Because not all mothers know their PEMT or MTHFR1 gene status supplementing with choline during pregnancy at approximately 980 mg per day, as was done in the study above, may help to ensure adequate levels are available for proper infant brain development. In addition, vegans are at high risk for being choline deficient and should definitely consider supplementing. Vegetarians who eat eggs daily are less likely to be deficient. One egg contains about 150 mg of choline.
Natural cholinesterase inhibitors
Because many people are looking to avoid the side effects from pharmaceutical cholinesterase inhibitors, natural cholinesterase inhibitors have grown in popularity in recent years. Using such compounds to address ACh deficiency does not address the root cause. The root cause of ACh deficiency is most often rooted in a deficiency in one or several of the precursors needed to make it. The preferred means to address ACh deficiency is to provide the body with necessary precursors in amounts that have been determined to be individual for each person based on diet, labs, history and symptoms. Using cholinesterase inhibitors can include side effects as it's interfering with the body's ability to naturally eliminate excess ACh when needed. I'll list a few of these compounds below, but want to highlight that root cause should be addressed first. In addition, when working with children it's important to use natural cholinesterase inhibitors with the fewest side effects and highest record for safety.
| Bacopa monnieri (also known as brahmi, water hyssop, and Herpestis monniera) is one of my favorite nootropic herbs. It has the lowest chance of creating side effects over other forms of cholinesterase inhibitors. "Emerging research demonstrates several mechanisms of action—acetylcholinesterase inhibition, choline acetyltransferase activation, b-amyloid reduction, increased cerebral blood flow, and monoamine potentiation." (Aguiar and Borowski, 2013) One side effect that is possible with Bacopa is loose stools. This is likely due to increased levels of ACh. The dose can be reduced if this occurs. However, Kumar, et al stated "Bacopa in syrup form, equivalent to 1 gm dried Bacopa daily, for three months in 40 school children aged 6–8 years, showed improvement in immediate memory, perception, and reaction performance without any side effects." (Kumar, 2016). |
Gotu Kola (also known as Centella asiatica) is another favorite nootropic herb of mine due to the research supporting it's efficacy and few reported side effects. "Several mechanisms of action of C. asiatica were demonstrated for enhancing cognitive function, such as the inhibition of acetylcholinesterase activity, reduction of phospholipase A2 (PLA2) activity, protection against ß-amyloid formation, and protection from brain damage." (Puttarak, 2017)
Gohil et al report "CA has no known toxicity in recommended doses. Side effects are rare but may include skin allergy and burning sensations (with external use), headache, stomach upset, nausea, dizziness, and extreme drowsiness which tend to occur with high doses of the herb." (Gohil, 2010)
Both Bacopa and Gotu Kola were used in a formula that was tested in children with ADHD. It was not only shown to be effective but "No serious adverse events were reported, and the rate of even mild adverse events among CHP-treated patients was actually less than that of placebo. (Katz, 2010). (CHP is compound herbal preparation.)
Gohil et al report "CA has no known toxicity in recommended doses. Side effects are rare but may include skin allergy and burning sensations (with external use), headache, stomach upset, nausea, dizziness, and extreme drowsiness which tend to occur with high doses of the herb." (Gohil, 2010)
Both Bacopa and Gotu Kola were used in a formula that was tested in children with ADHD. It was not only shown to be effective but "No serious adverse events were reported, and the rate of even mild adverse events among CHP-treated patients was actually less than that of placebo. (Katz, 2010). (CHP is compound herbal preparation.)
Huperzine A is extracted from Huperzia Serrata, a firmoss, which has been used for various diseases in traditional Chinese medicine for fever and inflammation. It has potent cholinesterase inhibition activity. (Wang, 2006) While it has been shown to be effective for improving memory due to mechanisms other than just cholinesterase inhibition (Zhang, 2008), it has not traditionally been used in children and no studies exist reporting it's efficacy or safety in children. Use in children has been deemed "possibly safe" when taken for less than one month. (WebMD)
Potential side effects include nausea, diarrhea, vomiting, sweating, blurred vision, slurred speech, restlessness, loss of appetite, contraction and twitching of muscle fibers, cramping, increased saliva and urine, inability to control urination, high blood pressure, and slowed heart rate. (WebMD)
For these reasons, along with focusing on addressing root cause, I don't typically recommend using Huperzine A in my patients.
Potential side effects include nausea, diarrhea, vomiting, sweating, blurred vision, slurred speech, restlessness, loss of appetite, contraction and twitching of muscle fibers, cramping, increased saliva and urine, inability to control urination, high blood pressure, and slowed heart rate. (WebMD)
For these reasons, along with focusing on addressing root cause, I don't typically recommend using Huperzine A in my patients.
Down Syndrome
Because choline has been shown to optimize brain development and methylation is necessary for optimal choline synthesis, choline supplementation in the Down syndrome model has been tested. Dr. Barbara Strupp and her team at Cornell University have done some very important and clinically relevant work in this area. They first wrote about the potential benefit of choline supplementation prenatally in pregnant mothers carrying an infant with Down syndrome in 2016. In this review article they explain the cognitive deficits related to cholinergic pathways in mice that are engineered to have an extra chromosome (Ts65Dn mice) that correlates with that in human trisomy 21. They stated, "Using the Ts65Dn mouse model of DS/AD, our group has identified a putative novel therapeutic intervention that holds great promise for improving cognitive outcome and offering neuroprotection to the cholinergic projection system in DS; namely, supplementing the maternal diet with additional choline during pregnancy and lactation." (Strupp, 2016)
They moved on in 2017 with researching actual maternal choline supplementation (MCS) in the Ts65Dn mouse model. They were able to state, "These results support the lifelong attentional benefits of MCS for Ts65Dn and 2N offspring and have profound implications for translation to human DS and pathology attenuation in AD." (Strupp, 2017)
In 1986 a report of supplementing phosphatidylcholine in a 2.5 year old child with Down syndrome was published. They reported no other supplements given. After 7 months "The child showed a definitive increase in speech and language skills as well as general motor skills which exceeded same aged Down Syndrome peers experiencing like training programs." (Cantor, 1986)
They moved on in 2017 with researching actual maternal choline supplementation (MCS) in the Ts65Dn mouse model. They were able to state, "These results support the lifelong attentional benefits of MCS for Ts65Dn and 2N offspring and have profound implications for translation to human DS and pathology attenuation in AD." (Strupp, 2017)
In 1986 a report of supplementing phosphatidylcholine in a 2.5 year old child with Down syndrome was published. They reported no other supplements given. After 7 months "The child showed a definitive increase in speech and language skills as well as general motor skills which exceeded same aged Down Syndrome peers experiencing like training programs." (Cantor, 1986)
| Thiamine supplementation at 50 mg given three times per day has also been shown to improve speech, mood, energy and cognition in adults with Down syndrome. (Reading, 1979) The mechanism behind these changes are likely due to an increase in ACh as well as the many other benefits thiamine supplementation provides. |
If you've given your child with Down syndrome a natural cholinesterase inhibitor and seen improvements in gross motor skills, cognition, speech and overall energy levels it's potentially related to an underlying deficiency that has not been properly addressed. This can happen even when giving a multivitamin that contains the cofactors necessary for ACh synthesis if the levels are not high enough for your child's specific needs or malabsorption has not been addressed. If an underlying deficiency goes undetected and untreated other biochemical needs of the body can go unaddressed. Thiamine deficiency, for example, is something I've detected in many of my patients with Down syndrome. It's function in ACh synthesis is just one of many ways thiamine supports brain function and overall health. Thiamine is essential for glucose metabolism, which must be optimized for proper brain function. Optimal glucose metabolism is needed in the brain for more than just ACh synthesis (Mergenthaler, 2013)
Steps to optimize ACh synthesis for your child
- Review signs and symptoms of ACh deficiency with their physician. Determine if need to support ACh synthesis exists.
- Test for B vitamin deficiencies using organic acid testing. Clues to B vitamin deficiencies can be seen in routine labs as elevated fasting blood sugar, low ferritin, elevated MCV, among others.
- Supplement with phosphatidylcholine, especially when eggs and meat are low in the diet
- Supplement with phosphatidylcholine if pregnant or breastfeeding, especially if following a vegan or vegetarian diet
- Supplement with appropriate levels of B vitamins specific for your child as indicated by test results
- Address underlying root cause for malabsorption of B vitamins. Organic acid testing and stool analysis can detect gastrointestinal issues contributing to malabsorption.
Remember, every child with Down syndrome is unique. Some may have a significant need for addressing ACh deficiency and some may not. "With full trisomy, intuitively it might be assumed that expression levels of triplicated genes are 1.5-fold that of the euploid population. However, this is not so." (Strydom, 2016)



 RSS Feed
RSS Feed