This question comes up a lot online: "What are the optimal reference ranges for thyroid hormone labs in children?" I hope this post serves to help parents and physicians understand optimal reference ranges for children versus reference ranges reported on actual lab results. This is an important topic as thyroid hormone is crucial for brain and global development of infants and children.
Unfortunately, there are no national or international standards for reference ranges that labs use. This has resulted in sometimes huge variations in reference ranges used by different labs. Ultimately, a well-studied physician should have their own reference ranges that they use when evaluating labs.
The six most important labs to obtain when assessing thyroid function, regardless of the age of the patient, are:
Unfortunately, there are no national or international standards for reference ranges that labs use. This has resulted in sometimes huge variations in reference ranges used by different labs. Ultimately, a well-studied physician should have their own reference ranges that they use when evaluating labs.
The six most important labs to obtain when assessing thyroid function, regardless of the age of the patient, are:
- TSH
- free T4
- free T3
- reverse T3
- TPO
- TgAb
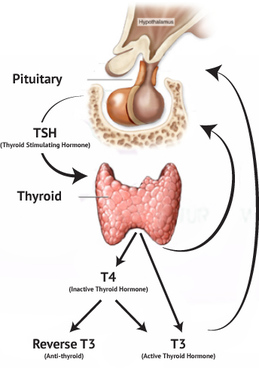
| TSH (thyroid stimulating hormone) is secreted from the pituitary gland. It's released into the blood stream where it travels to the thyroid gland. TSH docks with receptors on the thyroid gland, triggering the gland to secrete T4 (thyroxine) hormone. It also secretes some T3 (triiodothyronine) hormone. T4 and T3 are secreted in an 11:1 ratio (Snyder, 2012) from the thyroid gland in humans. T4 hormone travels from the thyroid gland back to the pituitary gland as well as throughout the whole body. The pituitary gland responds to levels of T4 in the blood by lowering TSH that is secreted, but not too much. A negative feedback loop is created that results in a stable release of TSH from the pituitary and T4 from the thyroid gland. T4 that travels througout the rest of the body must be converted to T3 hormone at the cellular level. T3 hormone is active thyroid hormone that every cell of the body is dependent upon to function. T4 converting to T3 hormone occurs when one iodine atom is removed from T4 to result in T3 hormone. |
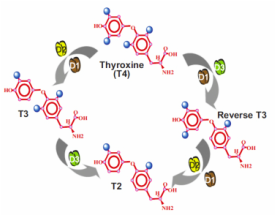
| This removal of iodine is accomplished by deiodinase enzymes (D1, D2 and D3 in Image 2). There are several forms of this enzyme. One form removes the iodine that results in active T3 hormone and and another form removes an iodine that results in inactive thyroid hormone called reverse T3. This is the body's system of "deciding" on a cellular level how much energy is needed in any given moment. When too much reverse T3 is generated compared to active T3 this results in hypothyroidism that goes by several names, Euthyroid Sick Syndrome or Non-thyroidal Illness Syndrome. (Lee, 2016; DeGroot, 2015) |
The most important message to take away from this is that the thyroid hormone process within the body is complicated and involves many steps that include proper pituitary function, thyroid gland function, deiodinase enzyme function, cell receptors and thyroid hormone receptors within each cell of the body. A problem in any of these steps can result in hypothyroidism.
Given the negative feedback loop that occurs between TSH and T4, endocrinologists have been using TSH levels only to assess the health of the very complicated thyroid hormone process for their patients. This has resulted in many patients who still experience symptoms of hypothyroidism but are told by their doctor that they don't have hypothyroidism. The result of this for an adult is often continued fatigue, depression, weight gain, dry skin and many other symptoms. Given the critical role thyroid hormone plays in childhood development at key stages that can't be revisited, this same incomplete assessment can result in irreversible lack of optimal brain development. For a thorough review of the important role thyroid hormone plays in brain development please read "Thyroid Hormones in Brain Development and Function" by Juan Bernal, M.D. Ph.D.
As it turns out several studies do exist supporting that the current practice of using TSH only to assess thyroid hormone function is missing a lot of patients with hypothyroidism, including children. One such study was conducted in 2005 by researchers at Athens University School of Medicine (Koutras, 2005). They tested TSH, T4 and T3 levels in 85 patients with hypothyrodism who were taking T4-only medication. They found that these patients had lower T3 levels compared to normal, non-hypothyroid subjects. They concluded that hypothyroid patients may benefit from co-administration of T3 and T4 medication. They also concluded, "TSH levels used to monitor substitution, mostly regulated by intracellular T3 in the pituitary, may not be such a good indicator of adequate thyroid hormone action in all tissues. " In 2015 a team of physicians collaborated to write "Homeostatic Control of the Thyroid–Pituitary Axis: Perspectives for Diagnosis and Treatment". They suggest that the use of TSH be "scaled back" and highlight the importance of T3 hormone levels.
The most important work being done to support the need to use more in-depth labs and assessment when testing patients for hypothyroidism is Dr. Antonio Bianco. The website for his lab is Deiodinase.org. His lab is doing extensive and valuable work investigating the important role that local cellular control of thyroid hormone plays in the thyroid status of patients. This website contains a wealth of knowledge regarding deiodinase enzymes and I highly recommend Endocrinologists start studying his work.
Although the role TSH levels play in thyroid hormone assessment should be downplayed, an optimal reference range should still be discussed. Many functional medical doctors agree that an optimal reference range for a test result is quite different than reference ranges that have been established by labs. These reference ranges may be capturing lab values for patients with undiagnosed pathology. The optimal reference range for TSH is generally accepted to be 1.0-2.5 mIU/L. In 2015 the American Association of Clinical Chemistry published "Thyroid-Stimulating Hormone" in which they state:
Given the negative feedback loop that occurs between TSH and T4, endocrinologists have been using TSH levels only to assess the health of the very complicated thyroid hormone process for their patients. This has resulted in many patients who still experience symptoms of hypothyroidism but are told by their doctor that they don't have hypothyroidism. The result of this for an adult is often continued fatigue, depression, weight gain, dry skin and many other symptoms. Given the critical role thyroid hormone plays in childhood development at key stages that can't be revisited, this same incomplete assessment can result in irreversible lack of optimal brain development. For a thorough review of the important role thyroid hormone plays in brain development please read "Thyroid Hormones in Brain Development and Function" by Juan Bernal, M.D. Ph.D.
As it turns out several studies do exist supporting that the current practice of using TSH only to assess thyroid hormone function is missing a lot of patients with hypothyroidism, including children. One such study was conducted in 2005 by researchers at Athens University School of Medicine (Koutras, 2005). They tested TSH, T4 and T3 levels in 85 patients with hypothyrodism who were taking T4-only medication. They found that these patients had lower T3 levels compared to normal, non-hypothyroid subjects. They concluded that hypothyroid patients may benefit from co-administration of T3 and T4 medication. They also concluded, "TSH levels used to monitor substitution, mostly regulated by intracellular T3 in the pituitary, may not be such a good indicator of adequate thyroid hormone action in all tissues. " In 2015 a team of physicians collaborated to write "Homeostatic Control of the Thyroid–Pituitary Axis: Perspectives for Diagnosis and Treatment". They suggest that the use of TSH be "scaled back" and highlight the importance of T3 hormone levels.
The most important work being done to support the need to use more in-depth labs and assessment when testing patients for hypothyroidism is Dr. Antonio Bianco. The website for his lab is Deiodinase.org. His lab is doing extensive and valuable work investigating the important role that local cellular control of thyroid hormone plays in the thyroid status of patients. This website contains a wealth of knowledge regarding deiodinase enzymes and I highly recommend Endocrinologists start studying his work.
Although the role TSH levels play in thyroid hormone assessment should be downplayed, an optimal reference range should still be discussed. Many functional medical doctors agree that an optimal reference range for a test result is quite different than reference ranges that have been established by labs. These reference ranges may be capturing lab values for patients with undiagnosed pathology. The optimal reference range for TSH is generally accepted to be 1.0-2.5 mIU/L. In 2015 the American Association of Clinical Chemistry published "Thyroid-Stimulating Hormone" in which they state:
| Although there is a consensus that the lower limit of the euthyroid reference interval for TSH should be 0.2–0.4 mIU/L, experts disagree about the appropriate upper limit. In 2002, researchers published an analysis of thyroid function test results from a large survey of individuals representative of the U.S. population (3). The study revealed that within a small standard error the mean TSH level in the general population is approximately 1.5 mIU/L. This finding prompted organizations to call for lowering the upper limit of the normal TSH reference range. The National Academy of Clinical Biochemistry recommended 4 mIU/L, while the American Association of Clinical Endocrinologists set the upper limit at 3 mIU/L, and other groups went as low as 2.5 mIU/L |
As well, researchers in the UK refer to a normal TSH as <2 mIU/L in "Pitfalls in the measurement and interpretation of thyroid function test".
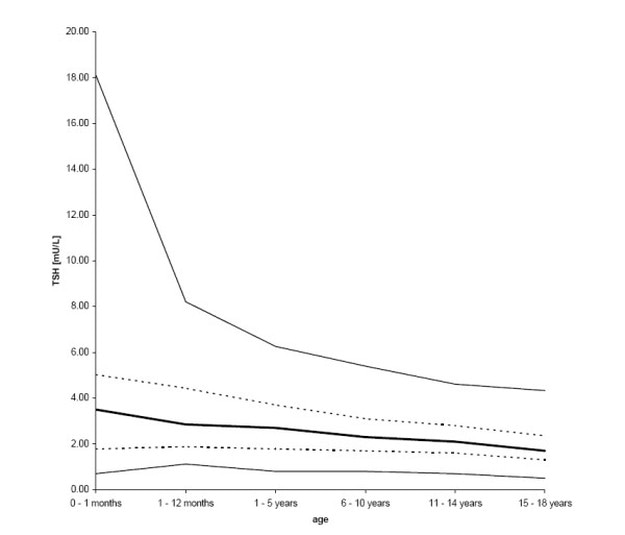
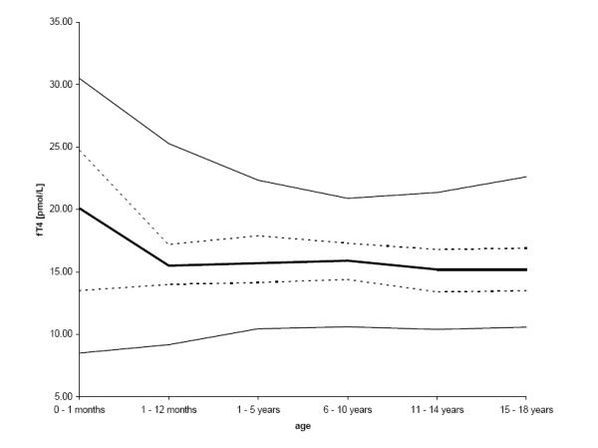
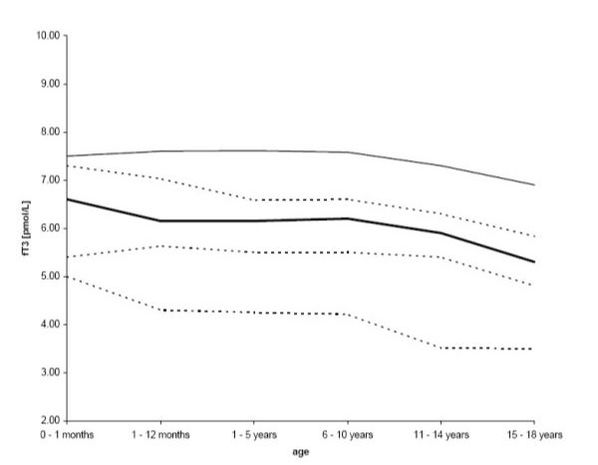
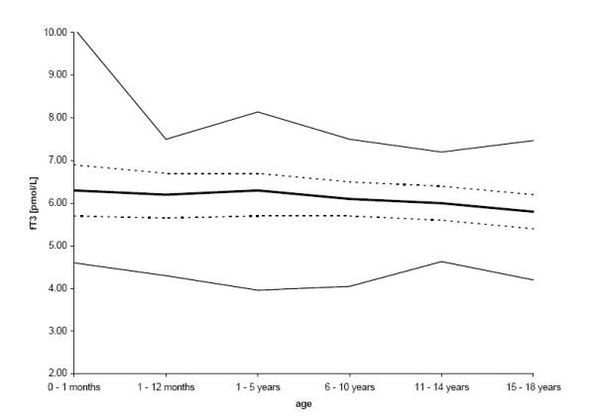
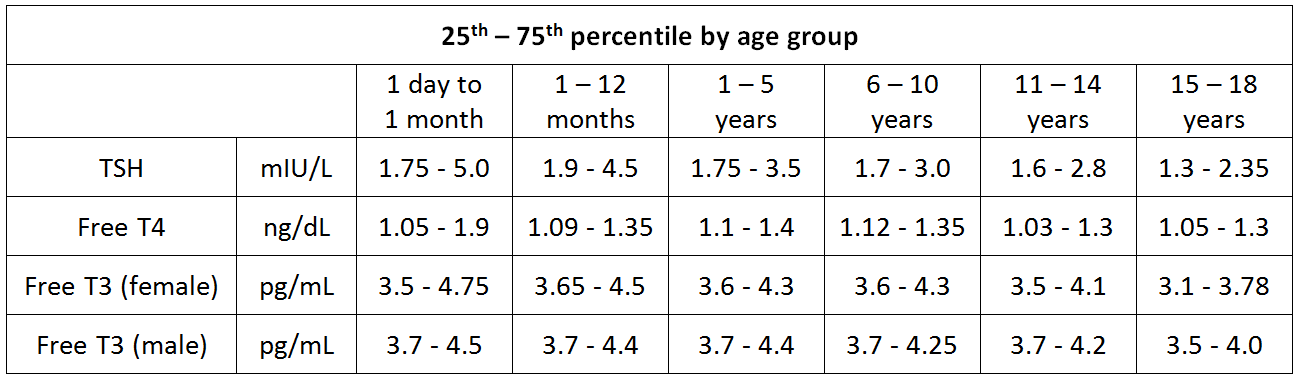
The optimal reference range for TSH in newborns, infants and children varies from those of adults. In addition, there are definite differences in optimal free T4 and free T3 levels in children. The most comprehensive anaylsis of thyroid hormone tests of pediatric patients was done in 2008 (Kapelari, 2008). Researchers analyzed medical records of 414 patients. Patients were grouped into age ranges of 1 day to 1 month, 1 – 12 months, and 1 – 5, 6 – 10, 11 – 14, and 15 – 18 years, respectively. They state in their conclusion, "Our results corroborate those of previous studies showing that thyroid hormone levels change markedly during childhood, and that adult reference intervals are not universally applicable to children." The images below are graphs from this study displaying their findings. The darkest black line in the graphs represents the 50th percentile (median) lab result.
The optimal reference range for TSH in newborns, infants and children varies from those of adults. In addition, there are definite differences in optimal free T4 and free T3 levels in children. The most comprehensive anaylsis of thyroid hormone tests of pediatric patients was done in 2008 (Kapelari, 2008). Researchers analyzed medical records of 414 patients. Patients were grouped into age ranges of 1 day to 1 month, 1 – 12 months, and 1 – 5, 6 – 10, 11 – 14, and 15 – 18 years, respectively. They state in their conclusion, "Our results corroborate those of previous studies showing that thyroid hormone levels change markedly during childhood, and that adult reference intervals are not universally applicable to children." The images below are graphs from this study displaying their findings. The darkest black line in the graphs represents the 50th percentile (median) lab result.
The conversion of pmol/L to pg/mL, the unit of measurement most often used in the US for free T3, uses the conversion factor of 1.536. The pmol/L number is divided by 1.536 to get pg/mL. The conversion of pmol/L to ng/dL, the unit of measurement most often used in the US for free T4, uses the conversion factor of 12.9. The pmol/L number is divided by 12.9 to get ng/dL.
The results from Kapelari's study are converted to US units of measurement and summarized in Table 1.
The results from Kapelari's study are converted to US units of measurement and summarized in Table 1.
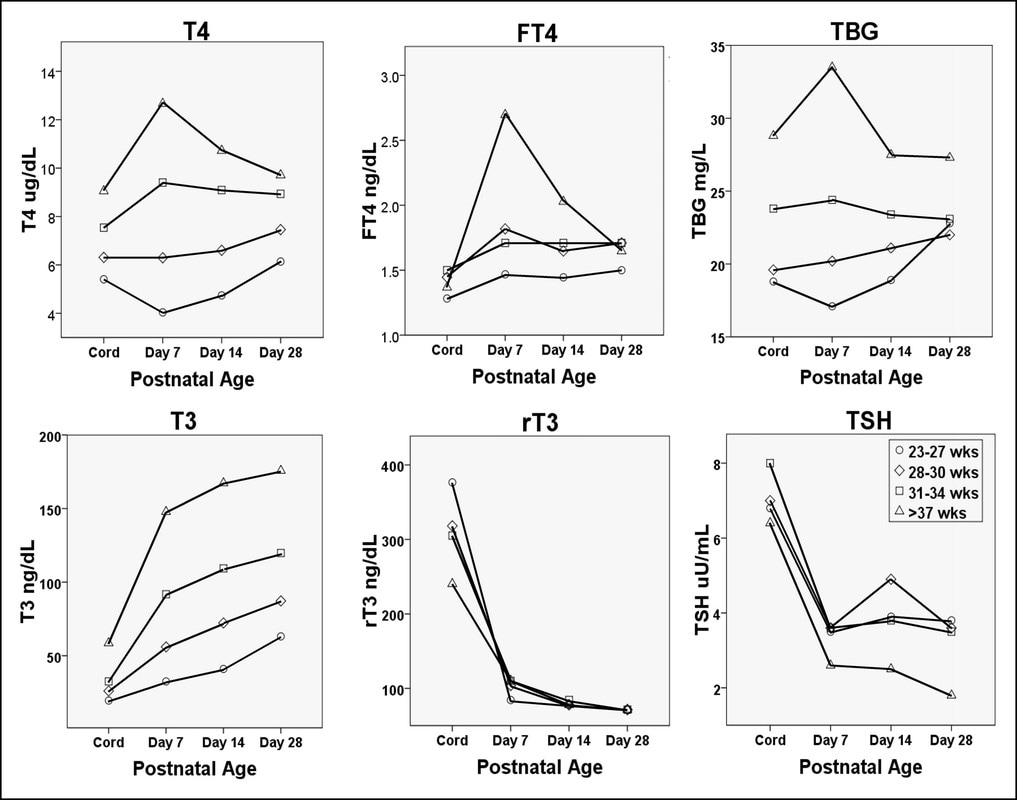
A reference range for reverse T3 in infants and children has not yet been established nor has it adequately been studied. However, some studies do exist. Researchers at UCLA studied levels of T4, T3 and reverse T3 in neonates from 1-30 days old. They found that "high serum rT3 concentration in the newborn becomes comparable to that in the normal adult by 9-11 days of neonatal life." (Chopra, 1975) The same dramatic decrease in reverse T3 in newborns was reported by Dr. Brown and Feingold in 2010 as seen in Image 7. (Brown, 2010) A striking increase in T3 levels after birth was noted by both studies as well. Reference range for reverse T3 in adults has been established to be 10-24 ng/dL. (Endocrine Society Laboratory Reference Ranges) Unfortunately, until further studies are conducted the only information available today regarding reverse T3 in infants is to use that of adults.
It's of utmost importance to assess signs and symptoms of hypothyroidism in infants and children in addition to lab results when determining their thyroid hormone status and whether thyroid hormone supplementation is warranted or not. Those signs and symptoms include:
- Dull look
- Puffy face
- Thick, protruding tongue
- Choking episodes
- Constipation
- Dry, brittle hair
- Jaundice
- Low muscle tone (floppy infant)
- Low hairline
- Poor feeding
- Short height
- Sleepiness
- Sluggishness
- Slow growth
- Hoarse-sounding cry or voice
- Short arms and legs
- Very large soft spots on the skull (fontanelles)
- Wide hands with short fingers
Thyroid antibodies should always be checked when assessing thyroid status given the high prevalence of autoimmune induced hypothyroidism. Naturally, these antibodies ideally should be as low as possible. Once again reference ranges vary widely from lab to lab. The Endocrine Society has determined the reference range for thyroid antibodies to be:
- TPO (Thyroperoxidase) - < 2.0 IU/mL
- TgAb (Thyroglobulin antibodies) - < 4.0 IU/mL
In short, hypothyroidism should not be missed in any infant or child given the important role thyroid hormone plays in the health and development of children. Signs and symptoms should never be ignored and a complete and thorough check of all thyroid hormone levels should be conducted.
**Please do not write comments that include your child's specific lab values asking for medical advise. We will not be able to give medical advise based on lab values alone and cannot give medical advise in this format. These comments will not be approved for posting. Feel free to contact the office to make an appointment if you would like our help.


 RSS Feed
RSS Feed