WARNING: The Federal Trade Commission mandates that prior to openly discussing any issues related to COVID 19 the following disclaimer be conspicuously placed in front of any article relating to COVID 19:
By now most of us have heard of coronavirus or COVID-19. If you don't know, the World Health Organization (WHO) announced it is officially a pandemic as of March 11, 2020. Does that mean we should panic? No. It means we should work even harder to ensure we and our children have a strong, healthy immune system. You may have heard that the coronavirus is a mild infection for young, healthy individuals and those who are experiencing more serious respiratory consequences and even death are those who are elderly and have some underlying health condition(s) that lead to the increased complications. Are children with Down syndrome among that group? It's definitely possible, but as of now, no reports of children or adults with Down syndrome contracting the virus have been reported. The risk factors for the increased rate of mortality in those who contracted coronavirus include:
This is according to a report published March 11, 2020 in the Lancet (Zhou 2020). Looking further at their data, we can see the lab findings of the non-survivors are also notable. They revealed a low lymphocyte count, high lactate dehydrogenase, higher creatine kinase than survivors, high hs-CRP, higher d-dimer than survivors, high ferritin and higher Il-6 than survivors. Several of these lab findings point to increased inflammation (ferritin, hs-CRP and IL-6). As well, a high lactate dehydrogenase denotes damaged tissues that have spilled their contents into the bloodstream.
Should we take extra precautions with children with Down syndrome during this pandemic, keeping them away from big events, public places, and definitely away from those with a fever or cough? Well, yes, especially for some of them. Only take your child to a hospital or clinic if absolutely necessary. I'll explain why and what we can do specifically for our children with Down syndrome that may result in a better outcome if they were to be exposed to COVID-19.
It was announced in 2017 that Down syndrome could be re-categorized as an immune system disorder (Green 2017) based on new research that showed elevated levels of pro-inflammatory cytokines, IL-6, MCP-1, IL-22 and TNF-α seen in blood samples of 165 individuals with Down syndrome. As with many studies, the researchers placed blame entirely on the presence of the extra chromosome despite saying "most of the proteome changes observed in people with DS correspond to proteins encoded elsewhere in the genome". What this means is the proteins involved in the immune changes seen were not even encoded by chromosome 21. This research left parents even more worried, with no explanation of why this occurred or how to help their children. Research like this that implies the only aspect of physiology that is impacting the health of those with Down syndrome is their extra chromosome isn't seeing the forest for the trees. I'll explain below the other factors that can increase these inflammatory cytokines.
GUT HEALTH
In our clinical experience, many children and adults with Down syndrome have gastrointestinal issues that can increase these same pro-inflammatory cytokines listed above. Those gastrointestinal issues include irritable bowel syndrome, candida overgrowth, small intestinal bacterial overgrowth and microbiome dysbiosis. All of these gastrointestinal conditions have revealed a similar pattern of increased inflammatory cytokines seen in the 2017 study. (Schirmer 2016, Kumamoto 2011, Steele 2001, Komatsu 2001, Li 2017). A team of gastroenterologists in Spain reported inflammatory bowel disease in three patients with Down syndrome and discussed the possible connection between these two conditions. (Souto-Rodríguez 2014) Optimizing gastrointestinal microbiome, reducing gastrointestinal inflammation and optimizing gut motility could lead to a reduction in the immune dysfunction often seen in those with Down syndrome. You can read Gut Motility - Driver of the Microbiome for more information about how to optimize gut motility. To reduce gut inflammation we often recommend a gluten-free, dairy-free diet for all of our patients with Down syndrome. "Patients on a GCD (gluten-containing diet) had more bowel movements per day, greater intestinal permeability, and greater inflammatory cytokine levels compared to patients on a GFD (gluten-free diet)." (Niland and Cash 2018)
Supporting all aspects of gut health is beyond the scope of this article. We recommend that parents not ignore symptoms of gastrointestinal inflammation as simply expected in those with Down syndrome but explore ways to optimize gut health. These symptoms include:
At the very least, if you've been considering a gluten-free/dairy-free diet for your child with Down syndrome now is the time. An anti-inflammatory diet that includes foods contained in the image below can be very healing for the gut as well.
- NONE OF THE PRODUCTS DISCUSSED IN THIS ARTICLE HAVE BEEN PROVEN IN DOUBLE BLIND PLACEBO STUDIES TO CURE PREVENT OR TREAT COVID 19. THE SCIENTIFIC ARTICLES SUPPORTING THE DISCUSSION OF THE EFFICACY OF TREATMENTS AND PRODUCTS RELATED TO COVID 19 ARE NOT DOUBLE BLIND PLACEBO STUDIES OF THE PRODUCT ITSELF.
- ACCORDING TO THE FTC, NO PRODUCT HAS BEEN PROVEN IN DOUBLE BLIND PLACEBO STUDIES TO PREVENT OR CURE COVID 19.
- THIS ARTICLE IS FOR INFORMATIONAL PURPOSES ONLY AND IT IS NOT INTENDED AS A REPLACEMENT FOR DIAGNOSIS OR TREATMENT BY YOUR DOCTOR.
By now most of us have heard of coronavirus or COVID-19. If you don't know, the World Health Organization (WHO) announced it is officially a pandemic as of March 11, 2020. Does that mean we should panic? No. It means we should work even harder to ensure we and our children have a strong, healthy immune system. You may have heard that the coronavirus is a mild infection for young, healthy individuals and those who are experiencing more serious respiratory consequences and even death are those who are elderly and have some underlying health condition(s) that lead to the increased complications. Are children with Down syndrome among that group? It's definitely possible, but as of now, no reports of children or adults with Down syndrome contracting the virus have been reported. The risk factors for the increased rate of mortality in those who contracted coronavirus include:
- Hypertension
- Diabetes
- Coronary Heart Disease
This is according to a report published March 11, 2020 in the Lancet (Zhou 2020). Looking further at their data, we can see the lab findings of the non-survivors are also notable. They revealed a low lymphocyte count, high lactate dehydrogenase, higher creatine kinase than survivors, high hs-CRP, higher d-dimer than survivors, high ferritin and higher Il-6 than survivors. Several of these lab findings point to increased inflammation (ferritin, hs-CRP and IL-6). As well, a high lactate dehydrogenase denotes damaged tissues that have spilled their contents into the bloodstream.
Should we take extra precautions with children with Down syndrome during this pandemic, keeping them away from big events, public places, and definitely away from those with a fever or cough? Well, yes, especially for some of them. Only take your child to a hospital or clinic if absolutely necessary. I'll explain why and what we can do specifically for our children with Down syndrome that may result in a better outcome if they were to be exposed to COVID-19.
It was announced in 2017 that Down syndrome could be re-categorized as an immune system disorder (Green 2017) based on new research that showed elevated levels of pro-inflammatory cytokines, IL-6, MCP-1, IL-22 and TNF-α seen in blood samples of 165 individuals with Down syndrome. As with many studies, the researchers placed blame entirely on the presence of the extra chromosome despite saying "most of the proteome changes observed in people with DS correspond to proteins encoded elsewhere in the genome". What this means is the proteins involved in the immune changes seen were not even encoded by chromosome 21. This research left parents even more worried, with no explanation of why this occurred or how to help their children. Research like this that implies the only aspect of physiology that is impacting the health of those with Down syndrome is their extra chromosome isn't seeing the forest for the trees. I'll explain below the other factors that can increase these inflammatory cytokines.
GUT HEALTH
In our clinical experience, many children and adults with Down syndrome have gastrointestinal issues that can increase these same pro-inflammatory cytokines listed above. Those gastrointestinal issues include irritable bowel syndrome, candida overgrowth, small intestinal bacterial overgrowth and microbiome dysbiosis. All of these gastrointestinal conditions have revealed a similar pattern of increased inflammatory cytokines seen in the 2017 study. (Schirmer 2016, Kumamoto 2011, Steele 2001, Komatsu 2001, Li 2017). A team of gastroenterologists in Spain reported inflammatory bowel disease in three patients with Down syndrome and discussed the possible connection between these two conditions. (Souto-Rodríguez 2014) Optimizing gastrointestinal microbiome, reducing gastrointestinal inflammation and optimizing gut motility could lead to a reduction in the immune dysfunction often seen in those with Down syndrome. You can read Gut Motility - Driver of the Microbiome for more information about how to optimize gut motility. To reduce gut inflammation we often recommend a gluten-free, dairy-free diet for all of our patients with Down syndrome. "Patients on a GCD (gluten-containing diet) had more bowel movements per day, greater intestinal permeability, and greater inflammatory cytokine levels compared to patients on a GFD (gluten-free diet)." (Niland and Cash 2018)
Supporting all aspects of gut health is beyond the scope of this article. We recommend that parents not ignore symptoms of gastrointestinal inflammation as simply expected in those with Down syndrome but explore ways to optimize gut health. These symptoms include:
- Bloating
- Constipation
- Nausea
- Reflux
- Low/high appetite
- Abdominal pain
- Poor weight gain or growth
At the very least, if you've been considering a gluten-free/dairy-free diet for your child with Down syndrome now is the time. An anti-inflammatory diet that includes foods contained in the image below can be very healing for the gut as well.
| HISTAMINE/MAST CELLS Mast cells are involved in the inflammation seen in those who contract coronavirus. "Coronavirus infection (regardless of the various types of corona virus) is primarily attacked by immune cells including mast cells (MCs)". (Conti 2020) These mast cells are located within the submucosa of the lungs and secrete histamine when triggered by infection. Histamine is an important part of the cascade of events that help our bodies fight infections. |
However, an excessive release of histamine will result in a stronger immune response and potentially increase the risk of mortality from a viral or bacterial infection. Individuals who are experiencing undiagnosed allergies or histamine intolerance (a reduced ability to clear histamine from the body) are likely to experience a stronger immune response to a viral or bacterial infection. In their review of the role that mast cells play in the immune response to Influenza A Graham, et al stated, "The literature review presented here shows the strong correlation between mast cell accumulation and degranulation at local sites of infection with the observed tissue damage and pathology, not only during highly pathological IAV infections but many other pathogenic viral infections of humans and animals. Additional studies examining other highly pathological viruses that are known to cause ARDS and/or vascular leakage are thus warranted, which would include the emerging coronaviruses..." They went on to say: "Overall, we hypothesize that excessive mast cell activation may be a common feature of highly pathological viral infections that cause ARDS and/or vascular leakage." (Graham 2015) ARDS is acute respiratory distress syndrome and is much more common in children with Down syndrome. (Bruijn 2007)
An easily reversible contributing factor to ARDS, in addition to histamine levels, is a low vitamin D level. Researchers at the University of Birmingham found that "vitamin D deficiency (levels below 20 ng/mL) is ubiquitous in patients with ARDS and relates to adverse outcome." (Dancer 2015) Low vitamin D levels are a common finding in children with Down syndrome. (Stagi 2015)
We have recently found elevated serum histamine levels in a majority of our patients with Down syndrome. The symptoms of elevated histamine are obvious in many and include chronic nasal congestion, skin rashes, irritability, trouble sleeping and brain fog. The mechanism of this elevated histamine can be explained by low s-adenosylmethionine (SAMe) levels along with gastrointestinal inflammation and increased gut permeability. (Ramsay 2010) SAMe is our body's main methyl donor needed by many biochemical processes to properly process neurotransmitters, hormones and clearing of histamine, to name a few. SAMe levels have been shown to be low in plasma of children with Down syndrome. (James 2001) Without enough SAMe, histamine levels will increase in the body, because the enzyme that clears histamine, histamine methyltransferase, is dependent on SAMEe donating a methyl group to function.
The underlying cause of low SAMe was postulated to be due to upregulation of the enzyme cystathionine β-synthase (CBS) whose gene is on chromosome 21. These same researchers tested the behavior of lymphocytes from these same patients in various medium that contained various nutrients shown to impact intermediates of the methylation cycle. They showed that methionine, methyl B12, and folinic acid all resulted in increased SAMe levels in lymphocyte cells obtained from children with Down syndrome.
The expression of the CBS gene and SAMe levels will vary for different children with Down syndrome as the genes on the extra chromosome are expressed differently for every child with Down syndrome. (Strydom 2016) As well, the cells of your child's body do not behave the same way lymphocytes do in a petri dish. There are many other factors that impact methylation outside of the extra chromosome including, but not limited to, diet, malabsorption of B vitamins and environment (mold and other toxins in the environment). It's important to assess the need for methylation support on an individual basis using labs that include:
Treatment will be based on individual results of the above tests. One way to support methylation safely is to provide the body with two compounds whose production within the body consumes a large amount of methyl groups. In fact, "The methylation of guanidinoacetate to form creatine consumes more methyl groups than all other methylation reactions combined." (Stead, 2001) Creatine is a compound that is essential for muscle energy production and low levels can cause low muscle tone. Checking creatinine levels before supplementing is best. If levels are low, which we often see, it's an indicator that methylation support is needed and supplementing with creatine can help. It should only be given to a child who is well-hydrated as creatine can draw water into muscle tissue and result in a headache for anyone who is dehydrated.
The second largest draw on methylation is the production of phosphatidylcholine. This is a phospholipid that's essential for cell membrane structure and bile viscosity. The choline it contains is a precursor to acetylcholine, a neurotransmitter needed for gut motility and skeletal muscle function. Providing the body with these two compounds can ease the load on methylation within the body, similar to easing the load on an engine. This will allow the body to use methyl groups for other biochemical processes like clearing histamine.
Quercetin is a very powerful, natural antihistamine that can be helpful for those with elevated histamine levels. It also has neuroprotective, anti-carcinogenic, anti-inflammatory and antiviral properties. (Li 2016, Cost 2016) It's been shown to reduce the duration of upper respiratory tract infections in middle aged and older individuals. (Heinz 2010) A meta-analysis of the effect of quercetin and other flavonoids on upper respiratory tract infections and overall immune function that included 14 studies stated, "These findings suggest that flavonoids are a viable supplement to decrease URTI incidence in an otherwise healthy population." (Somerville 2016) Given the mast cell involvement of coronavirus, the use of quercetin as a natural antihistamine is a safe and potentially protective intervention.
An easily reversible contributing factor to ARDS, in addition to histamine levels, is a low vitamin D level. Researchers at the University of Birmingham found that "vitamin D deficiency (levels below 20 ng/mL) is ubiquitous in patients with ARDS and relates to adverse outcome." (Dancer 2015) Low vitamin D levels are a common finding in children with Down syndrome. (Stagi 2015)
We have recently found elevated serum histamine levels in a majority of our patients with Down syndrome. The symptoms of elevated histamine are obvious in many and include chronic nasal congestion, skin rashes, irritability, trouble sleeping and brain fog. The mechanism of this elevated histamine can be explained by low s-adenosylmethionine (SAMe) levels along with gastrointestinal inflammation and increased gut permeability. (Ramsay 2010) SAMe is our body's main methyl donor needed by many biochemical processes to properly process neurotransmitters, hormones and clearing of histamine, to name a few. SAMe levels have been shown to be low in plasma of children with Down syndrome. (James 2001) Without enough SAMe, histamine levels will increase in the body, because the enzyme that clears histamine, histamine methyltransferase, is dependent on SAMEe donating a methyl group to function.
The underlying cause of low SAMe was postulated to be due to upregulation of the enzyme cystathionine β-synthase (CBS) whose gene is on chromosome 21. These same researchers tested the behavior of lymphocytes from these same patients in various medium that contained various nutrients shown to impact intermediates of the methylation cycle. They showed that methionine, methyl B12, and folinic acid all resulted in increased SAMe levels in lymphocyte cells obtained from children with Down syndrome.
The expression of the CBS gene and SAMe levels will vary for different children with Down syndrome as the genes on the extra chromosome are expressed differently for every child with Down syndrome. (Strydom 2016) As well, the cells of your child's body do not behave the same way lymphocytes do in a petri dish. There are many other factors that impact methylation outside of the extra chromosome including, but not limited to, diet, malabsorption of B vitamins and environment (mold and other toxins in the environment). It's important to assess the need for methylation support on an individual basis using labs that include:
- histamine, whole blood or plasma
- CBC (basophil count, MCV)
- homocysteine
- serum B12
- serum creatinine
- organic acid test
- Genova Diagnostic's Methylation Panel
Treatment will be based on individual results of the above tests. One way to support methylation safely is to provide the body with two compounds whose production within the body consumes a large amount of methyl groups. In fact, "The methylation of guanidinoacetate to form creatine consumes more methyl groups than all other methylation reactions combined." (Stead, 2001) Creatine is a compound that is essential for muscle energy production and low levels can cause low muscle tone. Checking creatinine levels before supplementing is best. If levels are low, which we often see, it's an indicator that methylation support is needed and supplementing with creatine can help. It should only be given to a child who is well-hydrated as creatine can draw water into muscle tissue and result in a headache for anyone who is dehydrated.
The second largest draw on methylation is the production of phosphatidylcholine. This is a phospholipid that's essential for cell membrane structure and bile viscosity. The choline it contains is a precursor to acetylcholine, a neurotransmitter needed for gut motility and skeletal muscle function. Providing the body with these two compounds can ease the load on methylation within the body, similar to easing the load on an engine. This will allow the body to use methyl groups for other biochemical processes like clearing histamine.
Quercetin is a very powerful, natural antihistamine that can be helpful for those with elevated histamine levels. It also has neuroprotective, anti-carcinogenic, anti-inflammatory and antiviral properties. (Li 2016, Cost 2016) It's been shown to reduce the duration of upper respiratory tract infections in middle aged and older individuals. (Heinz 2010) A meta-analysis of the effect of quercetin and other flavonoids on upper respiratory tract infections and overall immune function that included 14 studies stated, "These findings suggest that flavonoids are a viable supplement to decrease URTI incidence in an otherwise healthy population." (Somerville 2016) Given the mast cell involvement of coronavirus, the use of quercetin as a natural antihistamine is a safe and potentially protective intervention.
LYMPHOPENIA
A low lymphocyte count (lymphopenia) is a common finding in those with Down syndrome. (de Hingh 2005). Recall from above the lymphopenia seen in the non-survivors of the coronavirus. Because of this, I highly recommend parents and caregivers of those with Down syndrome obtain a current CBC that contains an absolute, not just a relative, lymphocyte count. If doing so, I recommend using anti-infective precautions (mask, wiping surfaces with disinfectant, not using the bathroom, etc.) when entering the clinic or phlebotomy center for the blood draw. If a CBC has been done within the last three months and there have been no significant changes to their health, this would suffice.
There are several causes for lymphopenia that can be remedied outside of it simply being due to the extra chromosome. We don't see lymphopenia in all of our patients with Down syndrome; therefore, it's likely due to some factor outside of the extra chromosome. Causes of lymphopenia include:
GLUCOSE METABOLISM
Glucose metabolism refers to the means by which cells obtain energy from glucose that is consumed through our diet. The simple act of eating food that contains glucose, whether it be from an apple, carrot or cookie does not guarantee that glucose will be converted to energy. There are many steps involved in converting glucose to energy. The most notable factor involved in this conversion is the presence of B vitamins. They are essential, not just supportive, to this process. This is important for the immune system, particularly lymphocytes, because they require energy from glucose to function properly.
In fact, glucose metabolism within lymphocytes has been shown to impact their function and survival. "Lymphocytes require glucose uptake and metabolism for normal survival and function." (MacIver 2008) Calculating a neutrophil: lymphocyte ratio has been shown to be a useful marker in assessing diabetic control. A higher ratio (due to a low lymphocyte count) may be indicative of impaired glucose metabolism. (Duman 2019) In addition, even short-term hyperglycemia has been shown to cause lymphopenia (Kanel 2001). High glucose in the blood is indicative of poor metabolism of glucose within the cell.
Glucose and carbohydrate metabolism has been studied in those with Down syndrome and shown to be impaired. (Labudova 1999, Pietrini 1997) Most of these studies focus on brain glucose metabolism, but the same mechanisms that impair glucose metabolism in the brain can also impact the rest of the body. A study looking at patients with ALL (Acute Lymphoblastic Leukemia) noted "Both hyperglycemia and infection were particularly common in patients with Down Syndrome." (Dare 2013)
A potential cause of impaired glucose metabolism is a deficiency of B vitamins. Malabsorption of B vitamins has been shown to occur in children with Down syndrome. (Abalan 1990) This has been our clinical experience as well. When we work to remedy malabsorption by improving gut motility and overall gut health, we see markers on organic acid testing indicating B vitamin deficiencies improve. Abalan, et al stated, "This hypothesis is supported by the description in DS of impaired digestive absorption of vitamin A, low blood levels of vitamin B1 despite adequate dietary intake and vitamin B1 supplements, and xylose excretion below normal after oral administration of a xylose load. This hypothesis could also explain the other signs of malnutrition observed in DS: red-cell folate values in the deficient range, unusual susceptibility to infections, depressed reactivity to skin tests antigens, impaired neutrophil bactericidal capacity, decreased responsiveness of lymphocytes to mitogens, and decreased capability of peripheral blood T lymphocytes to form rosettes with sheep red blood cells."
The deficiency mentioned here that's most remarkable and relates to glucose metabolism is vitamin B1 (thiamine). Thiamine is considered to be the most important B vitamin in the metabolism of glucose. Other B vitamins are necessary for glucose metabolism, but thiamine is needed at the "gateway" of the Citric Acid Cycle, which is an important step in generating energy from glucose. For more information on the role that thiamine plays in glucose metabolism you can watch the video below.
A low lymphocyte count (lymphopenia) is a common finding in those with Down syndrome. (de Hingh 2005). Recall from above the lymphopenia seen in the non-survivors of the coronavirus. Because of this, I highly recommend parents and caregivers of those with Down syndrome obtain a current CBC that contains an absolute, not just a relative, lymphocyte count. If doing so, I recommend using anti-infective precautions (mask, wiping surfaces with disinfectant, not using the bathroom, etc.) when entering the clinic or phlebotomy center for the blood draw. If a CBC has been done within the last three months and there have been no significant changes to their health, this would suffice.
There are several causes for lymphopenia that can be remedied outside of it simply being due to the extra chromosome. We don't see lymphopenia in all of our patients with Down syndrome; therefore, it's likely due to some factor outside of the extra chromosome. Causes of lymphopenia include:
- vitamin B6 deficiency (Miller 1998)
- oxidative stress (Suerda 2012)
- viral or parasitic infection (Territo 2020)
- autoimmune disorders (Schulze-Koops 2004)
- stress/high cortisol (Zidar 2019)
- impaired glucose metabolism (MacIver 2008)
GLUCOSE METABOLISM
Glucose metabolism refers to the means by which cells obtain energy from glucose that is consumed through our diet. The simple act of eating food that contains glucose, whether it be from an apple, carrot or cookie does not guarantee that glucose will be converted to energy. There are many steps involved in converting glucose to energy. The most notable factor involved in this conversion is the presence of B vitamins. They are essential, not just supportive, to this process. This is important for the immune system, particularly lymphocytes, because they require energy from glucose to function properly.
In fact, glucose metabolism within lymphocytes has been shown to impact their function and survival. "Lymphocytes require glucose uptake and metabolism for normal survival and function." (MacIver 2008) Calculating a neutrophil: lymphocyte ratio has been shown to be a useful marker in assessing diabetic control. A higher ratio (due to a low lymphocyte count) may be indicative of impaired glucose metabolism. (Duman 2019) In addition, even short-term hyperglycemia has been shown to cause lymphopenia (Kanel 2001). High glucose in the blood is indicative of poor metabolism of glucose within the cell.
Glucose and carbohydrate metabolism has been studied in those with Down syndrome and shown to be impaired. (Labudova 1999, Pietrini 1997) Most of these studies focus on brain glucose metabolism, but the same mechanisms that impair glucose metabolism in the brain can also impact the rest of the body. A study looking at patients with ALL (Acute Lymphoblastic Leukemia) noted "Both hyperglycemia and infection were particularly common in patients with Down Syndrome." (Dare 2013)
A potential cause of impaired glucose metabolism is a deficiency of B vitamins. Malabsorption of B vitamins has been shown to occur in children with Down syndrome. (Abalan 1990) This has been our clinical experience as well. When we work to remedy malabsorption by improving gut motility and overall gut health, we see markers on organic acid testing indicating B vitamin deficiencies improve. Abalan, et al stated, "This hypothesis is supported by the description in DS of impaired digestive absorption of vitamin A, low blood levels of vitamin B1 despite adequate dietary intake and vitamin B1 supplements, and xylose excretion below normal after oral administration of a xylose load. This hypothesis could also explain the other signs of malnutrition observed in DS: red-cell folate values in the deficient range, unusual susceptibility to infections, depressed reactivity to skin tests antigens, impaired neutrophil bactericidal capacity, decreased responsiveness of lymphocytes to mitogens, and decreased capability of peripheral blood T lymphocytes to form rosettes with sheep red blood cells."
The deficiency mentioned here that's most remarkable and relates to glucose metabolism is vitamin B1 (thiamine). Thiamine is considered to be the most important B vitamin in the metabolism of glucose. Other B vitamins are necessary for glucose metabolism, but thiamine is needed at the "gateway" of the Citric Acid Cycle, which is an important step in generating energy from glucose. For more information on the role that thiamine plays in glucose metabolism you can watch the video below.
Thiamine supplementation in individuals with Down syndrome has been studied and found to improve mood, behavior, speech and overall energy levels. (Reading 1979) Despite the positive findings of this small case report of only three patients no follow up studies exist, unfortunately. We have seen many positive results when using vitamin B1 in the form of benfotiamine for our patients with Down syndrome. An increase in lymphocyte count is one of those positive results we've seen.
OXIDATIVE STRESS
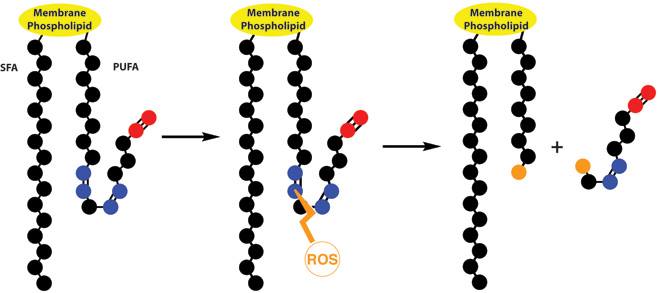
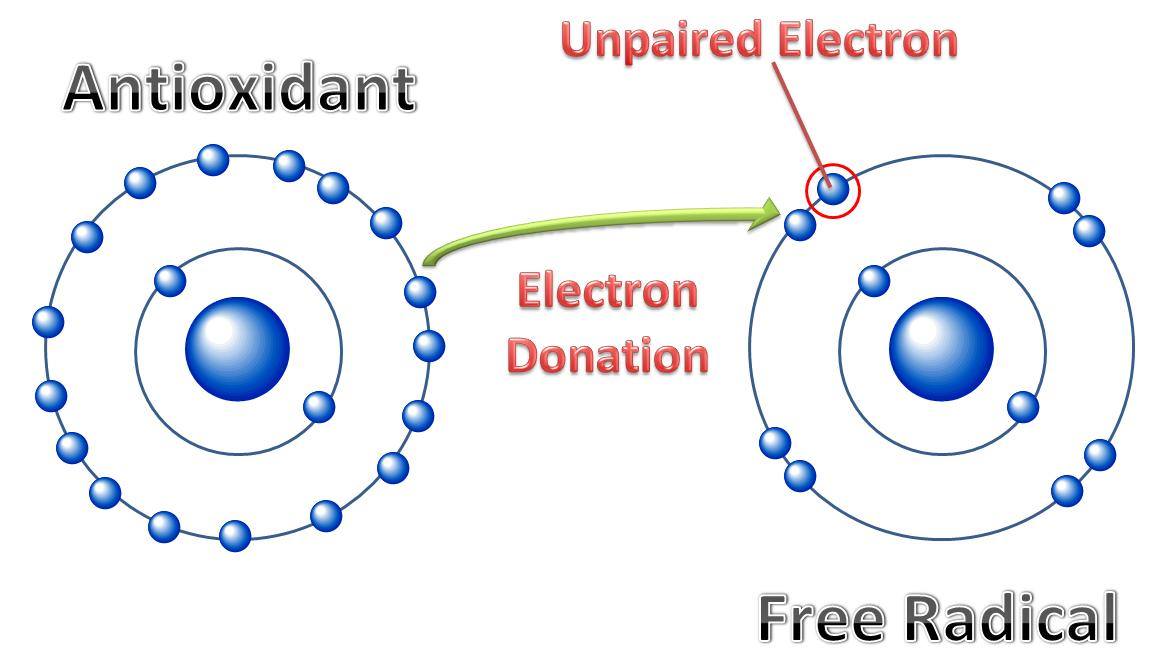
Reactive oxygen species (ROS) are chemically reactive oxygen molecules that cause cellular damage within the body known as oxidative stress. ROS are basically compounds that contain an unpaired electron. ROS are a normal byproduct of the energy production mechanisms that are constantly being produced within our cells. How well our body manages them is a major contributing factor to our overall health, including our immune system. "Oxidative stress contributes to many pathological conditions and diseases, including cancer, neurological disorders, atherosclerosis, hypertension, ischemia/perfusion, diabetes, acute respiratory distress syndrome, idiopathic pulmonary fibrosis, chronic obstructive pulmonary disease, and asthma." (Birben 2012)
ROS are also useful for the body as they're generated by immune cells in order to fight infection. They're generated by mast cells and lymphocytes when activated. (Suzuki 2005)
Electrons always prefer to travel in pairs, so these ROS compounds will steal an electron from other sources within the body. These other sources of an electron are often cell membranes and DNA. In this way, ROS can weaken cell membranes by breaking the chains of the phospholipid that are the building blocks of the cell membrane.
Reactive oxygen species (ROS) are chemically reactive oxygen molecules that cause cellular damage within the body known as oxidative stress. ROS are basically compounds that contain an unpaired electron. ROS are a normal byproduct of the energy production mechanisms that are constantly being produced within our cells. How well our body manages them is a major contributing factor to our overall health, including our immune system. "Oxidative stress contributes to many pathological conditions and diseases, including cancer, neurological disorders, atherosclerosis, hypertension, ischemia/perfusion, diabetes, acute respiratory distress syndrome, idiopathic pulmonary fibrosis, chronic obstructive pulmonary disease, and asthma." (Birben 2012)
ROS are also useful for the body as they're generated by immune cells in order to fight infection. They're generated by mast cells and lymphocytes when activated. (Suzuki 2005)
Electrons always prefer to travel in pairs, so these ROS compounds will steal an electron from other sources within the body. These other sources of an electron are often cell membranes and DNA. In this way, ROS can weaken cell membranes by breaking the chains of the phospholipid that are the building blocks of the cell membrane.
These weakened cell membranes can occur in mast cells as well. When cell membranes in mast cells are weak mast cells will more easily degranulate, or release their stored histamine. ROS are also involved in triggering of the IgE receptors on the surface of mast cells. (Suzuki 2005) A team of researchers in Moscow State University also state, "Based on the currently available data, it is possible to make a well founded suggestion that ROS play an important role in the regulation of the best studied and, apparently, the most important for mast cell degranulation FcεRI signaling..." (Chelombitko, 2016)
Fortunately, oxidative stress is another physiological phenomenon that we can impact through diet and supplementation. Vitamin C is well-known by many as a "mast cell stabilizer". It works by acting as an electron donor to "satisfy" the need the free radical has for an extra electron before it can cause damage to cell membranes or DNA. "Administration of vitamin C opposes free radical production and decreases bronchial hypersensitivity, an effect mediated by mast cells." (Shaik 2016)
Fortunately, oxidative stress is another physiological phenomenon that we can impact through diet and supplementation. Vitamin C is well-known by many as a "mast cell stabilizer". It works by acting as an electron donor to "satisfy" the need the free radical has for an extra electron before it can cause damage to cell membranes or DNA. "Administration of vitamin C opposes free radical production and decreases bronchial hypersensitivity, an effect mediated by mast cells." (Shaik 2016)
Vitamin C can be taken orally as well as administered intravenously. "Infusing high dose intravenous vitamin C into this patient with virus-induced ARDS was associated with rapid resolution of lung injury with no evidence of post-ARDS fibroproliferative sequelae." (Fowler 2017) A clinical trial using intravenous vitamin C for the treatment of severe COVID-19 pneumonia opened February 11, 2020. The results have yet to be published. I suspect they will be positive. (Peng 2020)
I highly recommend seeking out intravenous vitamin C in the event of any serious viral respiratory infection. Many outpatient clinics run by functional or naturopathic doctors offer this practice in the US. As well, some hospital intensivists may be convinced to use it if provided with studies to support its use, like the one from Fowler, et al above. Taking oral vitamin C to prevent oxidative stress before a viral infection is a safe and potentially protective mechanism as well.
There are many other forms of antioxidants that help to reduce the negative impact of oxidative stress. Some key ones I'll recommend here include glutathione and, again, quercetin and flavonoids. Quercetin and glutathione work well together. "Animal and cell studies found that quercetin induces GSH synthesis." (Xu 2019) It works be regulating and balancing SOD and glutathione, ultimately reducing the effects of oxidative stress.
Using NAC (a precursor to glutathione) has been shown to improve patient outcome in those with ARDS. (Soltran-Sharifi 2007) Results of a clinical trial intensive care unit patients in TN found "...patients with ARDS have depressed plasma and red cell glutathione concentrations, that these levels are substantially increased by therapy with intravenous NAC and there are measurable clinical responses to treatment with regard to increased oxygen delivery, improved lung compliance and resolution of pulmonary oedema." (Bernard 1990) NAC can be used as a precursor to glutathione or glutathione levels can be increased directly by taking oral liposomal glutathione.
Glutathione is an important antioxidant to consider for those with Down syndrome because glutathione levels have been found to be low in children with Down syndrome. (Pastore 2003) Low glutathione levels can greatly contribute to the presence of ROS in the body that leads to immune system dysfunction and mast cell activation.
I highly recommend seeking out intravenous vitamin C in the event of any serious viral respiratory infection. Many outpatient clinics run by functional or naturopathic doctors offer this practice in the US. As well, some hospital intensivists may be convinced to use it if provided with studies to support its use, like the one from Fowler, et al above. Taking oral vitamin C to prevent oxidative stress before a viral infection is a safe and potentially protective mechanism as well.
There are many other forms of antioxidants that help to reduce the negative impact of oxidative stress. Some key ones I'll recommend here include glutathione and, again, quercetin and flavonoids. Quercetin and glutathione work well together. "Animal and cell studies found that quercetin induces GSH synthesis." (Xu 2019) It works be regulating and balancing SOD and glutathione, ultimately reducing the effects of oxidative stress.
Using NAC (a precursor to glutathione) has been shown to improve patient outcome in those with ARDS. (Soltran-Sharifi 2007) Results of a clinical trial intensive care unit patients in TN found "...patients with ARDS have depressed plasma and red cell glutathione concentrations, that these levels are substantially increased by therapy with intravenous NAC and there are measurable clinical responses to treatment with regard to increased oxygen delivery, improved lung compliance and resolution of pulmonary oedema." (Bernard 1990) NAC can be used as a precursor to glutathione or glutathione levels can be increased directly by taking oral liposomal glutathione.
Glutathione is an important antioxidant to consider for those with Down syndrome because glutathione levels have been found to be low in children with Down syndrome. (Pastore 2003) Low glutathione levels can greatly contribute to the presence of ROS in the body that leads to immune system dysfunction and mast cell activation.
ANTI-VIRALS
Again, there are many here that can be discussed, but two stand out that are specific to those with Down syndrome in light of coronavirus as well. Those are Vitamin A and glycyrrhizin.
VITAMIN A
The malabsorption study of children with Down syndrome cited above also reported vitamin A among the deficiencies seen. (Abalan 1990) Years later researchers in Spain stated "Children with DS between two and six years old show a significantly lower serum retinol." (Chávez 2010) Before considering vitamin A supplementation it's wise to get a blood test to check for a deficiency and discuss supplementation with a nutritionally trained physician. Overdosing of vitamin A is possible and toxic to the body. "Mental status changes are common following Vitamin A intoxication. In addition, there is a risk for seizures, headache, and blurred vision (due to elevated intracranial pressure). Chronic toxicity can lead to alopecia, anorexia, pruritus, dryness of mucous membranes, muscle and bone pain and hyperlipidemia." (Olson 2019)
Vitamin A given in safe doses can greatly enhance the body's immune response. It's been shown in animal studies to increase serum levels of IgG, IgM, and IgA. (Huang 2018) Levels of these immunoglobulins can be tested in humans, as we often do on our patients. We have found low levels of each of these immunoglobulins in our patients with Down syndrome to varying degrees in each of them.
A study of 2,774 children in Bogotá, Colombia found "Vitamin A and hemoglobin concentrations were inversely related to rates of morbidity in school-age children." (Thornton 2014) From a global perspective in light of the recent spread of COVID-19 it should be noted that vitamin A deficiency is a major public health problem around the world.(Timoneda 2018) This could likely contribute to more serious complications from COVID-19 in those who are vitamin A deficient given the important role that vitamin A plays in lung health.
LICORICE (GLYCYRRHIZIN) - EDITED 3/14/2020
Previously I wrote of the potential benefits of glycyrrhizin, the active constituent of licorice, due to its antiviral properties. As well researchers in Germany tested glycyrrhizin against two clinical isolates of coronavirus (FFM-1 and FFM-2) from patients with SARS. "glycyrrhizin was the most active in inhibiting replication of the SARS-associated virus." (Cinatl 2003) Other researchers in Germany confirmed their findings and stated, "Glycyrrhizin (GL) was shown to inhibit SARS-coronavirus (SARS-CoV) replication in vitro." (Hoever 2005)
In "Potential natural compounds for preventing 2019-nCoV infection" Chen and Du also discussed the use of glycyrrhizin. They pointed out that COVID-19 enters the host lung cells via ACE2 receptors on the surface of the cell. "Targeting ACE2 holds the promise for preventing 2019-nCoV infection." (Chen and Du 2020) They went on to add, "Given the low toxicity of glycyrrhizin, its anti-virus effects on SARS and its potential interaction with ACE2, it’s worthwhile to test its efficacy against 2019- nCoV infection." (Chen and Du 2020)
Despite this, I'm retracting my recommendation of glycyrrhizin based on information that was published February 29, 2020. A team of researchers and doctors in China reported low potassium levels, hypokalemia, being linked to severity of lab results in patients who contracted COVID-19. "Body temperature, CK, CK-MB, LDH, and CRP were significantly associated with the severity of hypokalemia (P<0.01). 93% of severe and critically ill patients had hypokalemia which was most common among elevated CK, CK-MB, LDH, and CRP." (Li 2020)
Glycyrrhizin can cause renal potassium loss and subsequent high blood pressure. (Allcock 2015) Given that hypertension is among the co-morbid conditions seen in non-survivors of this novel coronavirus infection, and low potassium is linked to severity of aberrant lab results, it would be wise to avoid glycyrrhizin at this time. It should also be noted that the papers from Chen and Du and Li, et al are in pre-print, which means they have not been peer-reviewed and should not be used to guide clinical practice.
SUMMARY OF TIPS TO DISCUSS WITH YOUR CHILD'S DOCTOR
Again, there are many here that can be discussed, but two stand out that are specific to those with Down syndrome in light of coronavirus as well. Those are Vitamin A and glycyrrhizin.
VITAMIN A
The malabsorption study of children with Down syndrome cited above also reported vitamin A among the deficiencies seen. (Abalan 1990) Years later researchers in Spain stated "Children with DS between two and six years old show a significantly lower serum retinol." (Chávez 2010) Before considering vitamin A supplementation it's wise to get a blood test to check for a deficiency and discuss supplementation with a nutritionally trained physician. Overdosing of vitamin A is possible and toxic to the body. "Mental status changes are common following Vitamin A intoxication. In addition, there is a risk for seizures, headache, and blurred vision (due to elevated intracranial pressure). Chronic toxicity can lead to alopecia, anorexia, pruritus, dryness of mucous membranes, muscle and bone pain and hyperlipidemia." (Olson 2019)
Vitamin A given in safe doses can greatly enhance the body's immune response. It's been shown in animal studies to increase serum levels of IgG, IgM, and IgA. (Huang 2018) Levels of these immunoglobulins can be tested in humans, as we often do on our patients. We have found low levels of each of these immunoglobulins in our patients with Down syndrome to varying degrees in each of them.
A study of 2,774 children in Bogotá, Colombia found "Vitamin A and hemoglobin concentrations were inversely related to rates of morbidity in school-age children." (Thornton 2014) From a global perspective in light of the recent spread of COVID-19 it should be noted that vitamin A deficiency is a major public health problem around the world.(Timoneda 2018) This could likely contribute to more serious complications from COVID-19 in those who are vitamin A deficient given the important role that vitamin A plays in lung health.
LICORICE (GLYCYRRHIZIN) - EDITED 3/14/2020
Previously I wrote of the potential benefits of glycyrrhizin, the active constituent of licorice, due to its antiviral properties. As well researchers in Germany tested glycyrrhizin against two clinical isolates of coronavirus (FFM-1 and FFM-2) from patients with SARS. "glycyrrhizin was the most active in inhibiting replication of the SARS-associated virus." (Cinatl 2003) Other researchers in Germany confirmed their findings and stated, "Glycyrrhizin (GL) was shown to inhibit SARS-coronavirus (SARS-CoV) replication in vitro." (Hoever 2005)
In "Potential natural compounds for preventing 2019-nCoV infection" Chen and Du also discussed the use of glycyrrhizin. They pointed out that COVID-19 enters the host lung cells via ACE2 receptors on the surface of the cell. "Targeting ACE2 holds the promise for preventing 2019-nCoV infection." (Chen and Du 2020) They went on to add, "Given the low toxicity of glycyrrhizin, its anti-virus effects on SARS and its potential interaction with ACE2, it’s worthwhile to test its efficacy against 2019- nCoV infection." (Chen and Du 2020)
Despite this, I'm retracting my recommendation of glycyrrhizin based on information that was published February 29, 2020. A team of researchers and doctors in China reported low potassium levels, hypokalemia, being linked to severity of lab results in patients who contracted COVID-19. "Body temperature, CK, CK-MB, LDH, and CRP were significantly associated with the severity of hypokalemia (P<0.01). 93% of severe and critically ill patients had hypokalemia which was most common among elevated CK, CK-MB, LDH, and CRP." (Li 2020)
Glycyrrhizin can cause renal potassium loss and subsequent high blood pressure. (Allcock 2015) Given that hypertension is among the co-morbid conditions seen in non-survivors of this novel coronavirus infection, and low potassium is linked to severity of aberrant lab results, it would be wise to avoid glycyrrhizin at this time. It should also be noted that the papers from Chen and Du and Li, et al are in pre-print, which means they have not been peer-reviewed and should not be used to guide clinical practice.
SUMMARY OF TIPS TO DISCUSS WITH YOUR CHILD'S DOCTOR
- Anti-inflammatory diet (gluten-free, dairy-free)
- No refined sugar, absolutely none at this time
- B vitamins as warranted and tolerated
- Vitamin D
- Vitamin C
- Quercetin
- Liposomal Glutathione
- Vitamin A (use with caution)
- Obtain current labs that include CBC, serum B12, serum vitamin A, histamine, glutathione, homocysteine and immunoglobulins. Discuss all potential causes of aberrant results with your child's physician.
- More tips on boosting the immune system can be found by reading Boosting Immunity: Functional Medicine Tips on Prevention & Immunity Boosting During the COVID-19 (Coronavirus) Outbreak
To date, there are no proven treatments that are effective against COVID-19. Many of the interventions discussed here do have research to support the means by which they may be effective at supporting the immune system for anyone who encounters the virus. This is only a sample, actually, of the many ways that we can support the immune system of our loved ones with Down syndrome. Assessing how to best support the immune system for those with or without Down syndrome on an individual basis is always ideal. The number one intervention is a healthy diet that's rich in colorful fruits and vegetables and low in refined sugar...because you can't out supplement a bad diet.
May we all be well ❤
May we all be well ❤



 RSS Feed
RSS Feed