Those are some strong words that likely got your attention whether you're a parent or a physician. Medical neglect typically refers to a parent who neglects to seek out professional help for their child who is in obvious need of medical attention. This is not the medical neglect to which I'm referring. I would like to broaden that term to include physicians. That's right. Physicians who took an oath to "do no harm" now work in a healthcare system that doesn't give them enough time to always fully help their patients. When the writing of a prescription replaces the doctor's role to get to the root cause of the problem and the patient can as a result experience negative side effects from an unnecessary prescription then this patient has experienced more harm than good from that appointment. The average time doctors spend with their patients has been estimated to range anywhere from seven to fifteen minutes.(1, 2) In some cases those fifteen minute appointments are for a new patient. How can a physician possibly review everything necessary in order to truly help their patients in this amount of time? I spend two hours (sometimes up to three hours if I have to) with a new patient. Follow up appointments are no shorter than thirty minutes and those are often rushed with everything that needs to be discussed.
I'll discuss here how this current medical system impacts children with Down syndrome and autism, but this extends to children with ADD/ADHD, anxiety, OCD, seizures, Sensory Processing Disorders and others.
The correct or polite term for this is actually "diagnostic overshadowing". This term was first used in 1982 by Dr. Steven Reiss a professor and researcher in clinical psychology at Ohio State University. Dr. Reiss originally used the term in relation to those with mental illness. It's used today in reference to those with a learning disability as well. Diagnostic overshadowing is defined as leaving co-existing conditions undiagnosed and untreated once a diagnosis is made of a major condition, such as autism or Down syndrome. Children whose medical needs are being ignored simply because they are intellectually different are experiencing neglect of their medical needs. I call it like I see it. If you've ever heard a doctor say, "Well, that's normal for Down syndrome." or "That's expected in a child with autism." that child is experiencing diagnostic overshadowing or medical neglect as I see it.
It's ultimately not the physician's fault when they work in a system that doesn't allow them enough time with their patients or if they simply haven't been trained in functional medicine which addresses the true underlying causes of ill health. However, when a parent reaches out for help by presenting a physician with information that can help their child, and then that physician dismisses the information and tells the parent that what their child is experiencing is normal and expected given their diagnosis THAT is medical neglect. One analogy would be if a patient had bone cancer and was experiencing pain and the doctors chose to not look for the cause of the pain because pain is expected in patients with bone cancer. What if the pain is from a fracture that can be seen by an x-ray and helped with a simple cast? If this sounds preposterous to you then it should be equally absurd that developmental delay and cognitive issues in people with Down syndrome are dismissed as well.
I'll discuss here how this current medical system impacts children with Down syndrome and autism, but this extends to children with ADD/ADHD, anxiety, OCD, seizures, Sensory Processing Disorders and others.
The correct or polite term for this is actually "diagnostic overshadowing". This term was first used in 1982 by Dr. Steven Reiss a professor and researcher in clinical psychology at Ohio State University. Dr. Reiss originally used the term in relation to those with mental illness. It's used today in reference to those with a learning disability as well. Diagnostic overshadowing is defined as leaving co-existing conditions undiagnosed and untreated once a diagnosis is made of a major condition, such as autism or Down syndrome. Children whose medical needs are being ignored simply because they are intellectually different are experiencing neglect of their medical needs. I call it like I see it. If you've ever heard a doctor say, "Well, that's normal for Down syndrome." or "That's expected in a child with autism." that child is experiencing diagnostic overshadowing or medical neglect as I see it.
It's ultimately not the physician's fault when they work in a system that doesn't allow them enough time with their patients or if they simply haven't been trained in functional medicine which addresses the true underlying causes of ill health. However, when a parent reaches out for help by presenting a physician with information that can help their child, and then that physician dismisses the information and tells the parent that what their child is experiencing is normal and expected given their diagnosis THAT is medical neglect. One analogy would be if a patient had bone cancer and was experiencing pain and the doctors chose to not look for the cause of the pain because pain is expected in patients with bone cancer. What if the pain is from a fracture that can be seen by an x-ray and helped with a simple cast? If this sounds preposterous to you then it should be equally absurd that developmental delay and cognitive issues in people with Down syndrome are dismissed as well.
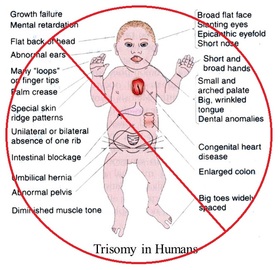
| Physicians are trained in outdated, inaccurate information about children with special needs. They're trained in what these children can't do and the negative aspects of the condition to look for when doing a physical exam. The image to the left is an example of something that might be seen in a medical textbook to explain what Down syndrome is. There's nothing in these textbooks that says anything about how many families feel blessed to have a child with Down syndrome and how much joy they bring to their lives. I've drawn a red "no" symbol over it because I hate to even include it in this article. It's merely an example. Physicians are not trained in the possibility that a child with special needs can overcome health challenges and that their potential is a lot more unlimited than history has deemed it to be. |
| What you won't see in medical textbooks are more accurate images like the one on the right. In fact, a recent survey of parents and siblings of those with Down syndrome found that 87% of them said their experience of having a family member with Down syndrome has been a positive one and almost as many said they felt pride for their child.(3) When a medical textbook paints the image of a child with Down syndrome, for example, as just a constellation of symptoms, organ dysfunction and cognitive delays how is a physician expected to know anything different? The truth is these children and adults often live vibrant, happy lives and contribute in immeasurable ways to their community and family. |
Some may be reading this and saying, "But what about those who are more severely affected?". I don't want to sugar coat it. Some children with Down syndrome and autism are more severely affected than others. However, these are the children and adults who most likely experienced medical neglect or diagnostic overshadowing during critical years of development that made the biggest impact on their health and cognition. If having an extra copy of chromosome 21 was the only thing that dictated the health and cognitive abilities of a person with Down syndrome how does one explain the large range of health and abilities in those with Down syndrome? Clearly their health and cognitive function must be impacted by more than just the extra chromosome.
I'll give you an example of a patient. I'll call her Mary in order to maintain anonymity and to give her a name instead of just calling her a "case". Mary was two years old when her mother brought her to see me. When I greeted them in the waiting room for the first time I immediately could see that Mary was not well. She did not make any eye contact, made few to no sounds, was extremely congested and could only roll around on the floor like a three month old. Mary's mother was told, "Well, she has Down syndrome." I can tell you right now that this was NOT "just Down syndrome." I've worked with hundreds of children with Down syndrome who were able to walk, talk and were quite engaging at her age.
Mary was diagnosed at birth with having Down syndrome and was her mother's third child. Despite being told that children with Down syndrome typically can't breastfeed and that she shouldn't even try, her mother was able to get her to exclusively breastfeed successfully for her first six months of life. Unfortunately at her six month checkup her Pediatrician realized she hadn't been growing. His means of managing this was to recommend that the mother stop breastfeeding and switch to commercial, powdered, dairy-based formula so that they could measure exactly how much Mary was actually feeding. Let's stop here. I hope you see that this was mistake #1. It has been well-established in medical literature that breast milk is best for babies.(4) One could argue that's it's even more important for a child with Down syndrome who is at greater risk for developmental delays and needs every advantage possible for optimal health. This physician chose to remove what was best for the child and ignore other possible causes of slow growth in children, one of which can be hypothyroidism which is very common in children with Down syndrome.
Mary had symptoms of hypothyroidism since birth that included low muscle tone, low temperature and prolonged jaundice, among others. Her thyroid labs were not checked at six months old when her growth was seen as an issue. Soon after starting formula she was also started on solids. Reflux and severe constipation, going as long as two weeks without a bowel movement, quickly became a problem after these changes to her diet. She was then put on Omeprazole at eight months old for the reflux. This is a medication that decreases acidity in the stomach and can lead to vitamin and mineral deficiencies. Studies show that dairy allergy is strongly linked to reflux in infants (5,6) and switching formula or finding a breast milk donor would have been the better choice.
I'll give you an example of a patient. I'll call her Mary in order to maintain anonymity and to give her a name instead of just calling her a "case". Mary was two years old when her mother brought her to see me. When I greeted them in the waiting room for the first time I immediately could see that Mary was not well. She did not make any eye contact, made few to no sounds, was extremely congested and could only roll around on the floor like a three month old. Mary's mother was told, "Well, she has Down syndrome." I can tell you right now that this was NOT "just Down syndrome." I've worked with hundreds of children with Down syndrome who were able to walk, talk and were quite engaging at her age.
Mary was diagnosed at birth with having Down syndrome and was her mother's third child. Despite being told that children with Down syndrome typically can't breastfeed and that she shouldn't even try, her mother was able to get her to exclusively breastfeed successfully for her first six months of life. Unfortunately at her six month checkup her Pediatrician realized she hadn't been growing. His means of managing this was to recommend that the mother stop breastfeeding and switch to commercial, powdered, dairy-based formula so that they could measure exactly how much Mary was actually feeding. Let's stop here. I hope you see that this was mistake #1. It has been well-established in medical literature that breast milk is best for babies.(4) One could argue that's it's even more important for a child with Down syndrome who is at greater risk for developmental delays and needs every advantage possible for optimal health. This physician chose to remove what was best for the child and ignore other possible causes of slow growth in children, one of which can be hypothyroidism which is very common in children with Down syndrome.
Mary had symptoms of hypothyroidism since birth that included low muscle tone, low temperature and prolonged jaundice, among others. Her thyroid labs were not checked at six months old when her growth was seen as an issue. Soon after starting formula she was also started on solids. Reflux and severe constipation, going as long as two weeks without a bowel movement, quickly became a problem after these changes to her diet. She was then put on Omeprazole at eight months old for the reflux. This is a medication that decreases acidity in the stomach and can lead to vitamin and mineral deficiencies. Studies show that dairy allergy is strongly linked to reflux in infants (5,6) and switching formula or finding a breast milk donor would have been the better choice.

Not long after being placed on Omeprazole she had what was interpreted as a seizure or infantile spasms. Sandifer's syndrome had not been ruled out. This is reflux that looks like a seizure and is under-recognized in the medical community. A short course of steroids was started to treat her "seizures" and was ineffective. Her seizure-like behavior/reflux was actually a sign that the Omeprazole was not working. Another sign that this medication was ineffective and that she was still experiencing reflux was her chronic upper respiratory congestion, a symptom of reflux. This congestion resulted in multiple rounds of antibiotics in her mere two years of life. Her adenoids were enlarged and removed at 18 months old after a sleep study was done that found moderate sleep apnea. This exposed her to anesthetics which can be harmful in a child who is not able to properly detox them from the body. In addition her pain after surgery was managed by multiple doses of Tylenol which has been shown to reduce the activity of the enzyme glutathione reductase. (7) This enzyme functions in a necessary step in our body's internal anti-oxidant and detoxification system and is crtical for children with Down syndrome.
Her extreme constipation and bloating resulted in a prescription for Miralax. It was advised that she take this daily for an extended period even though it's safety and use hasn't been studied in very young children. Many parents would be shocked to know, given how commonly Miralax is prescribed, that concerns over adverse side effects from it include seizures, tremors, tics, headache, anxiety, lethargy, sedation, aggression, rages, obsessive-compulsive behaviors including repetitive chewing and sucking, paranoia and mood swings." These side effects were discussed during the June 18, 2009 FDA Drug Safety Oversight Board meeting.(8)
Her extreme constipation and bloating resulted in a prescription for Miralax. It was advised that she take this daily for an extended period even though it's safety and use hasn't been studied in very young children. Many parents would be shocked to know, given how commonly Miralax is prescribed, that concerns over adverse side effects from it include seizures, tremors, tics, headache, anxiety, lethargy, sedation, aggression, rages, obsessive-compulsive behaviors including repetitive chewing and sucking, paranoia and mood swings." These side effects were discussed during the June 18, 2009 FDA Drug Safety Oversight Board meeting.(8)
You can imagine my frustration and sadness hearing her story. Misstep after misstep from well-intentioned, ill-informed doctors resulted in Mary's severe delay in development and probably contributed to much of her cognitive delays as well. At one point during her appointment, when the mother went outside to get some paperwork from her car, I picked up Mary to put her on my exam table. I looked at her closely and with great intention said, "We're going to get you back." I knew there was a lot I could do to help but was also fearful of the amount of damage that had been done.
I won't go into great detail about her treatment plan as that's outside the scope of this article. What I will say that I did was to treat her undiagnosed and untreated hypothyroidism, remove her from cow dairy formula and gave the mom some safe and very effective remedies for constipation, among other things. At her follow up appointment two months later I got to meet Mary for what seemed like the first time. She was alert, made eye contact (although infrequently), was able to sit up on her own for extended periods of time and she imitated me making some popping noises with my mouth. This was a huge leap in her development in only two months! We still have a lot of work to do to help Mary heal. Much of that work will be to heal her gut after the assault from dairy formula, Omeprazole, Miralax and antibiotics.
Mary's story is not unique. This happens to hundreds and thousands of children with special needs who experience more visits to the doctor's office than other children. These visits often result in prescriptions that are causing more harm than good, not to mention the lack of addressing the root cause of their symptoms. I recognize Mary's delays as being due to hypothyroidism and severe gastrointestinal dysbiosis NOT her having Down syndrome. Addressing hypothyroidism, gut dysbiosis and malabsorption are the biggest ways that children with Down syndrome and other special needs can be helped. Ignoring that environmental factors like mode of delivery, breastfeeding, diet, early exposure to antibiotics and other drugs that impact the microbiome have an even greater role on their health than that extra copy of chromosome 21 is the greatest medical tragedy that these children experience. Dr. Noel Mueller and his colleagues accurately stated "The infant microbiome plays an essential role in human health and its assembly is determined by maternal-offspring exchanges of microbiota. This process is affected by several practices, including Cesarean section (C-section), perinatal antibiotics, and formula feeding, that have been linked to increased risks of metabolic and immune diseases." in their 2015 review article.(9) In addition, it's been well established that children with autism have a greater prevalence of gastrointestinal problems than their typical peers as outlined in "Gastrointestinal Symptoms in Autism Spectrum Disorder: A Meta-analysis". (10) Many believe, given the strong connection between the health of the gut and the health of the brain, that this may be a major causative factor of autism.
The amount of research connecting the impact that our microbiome has on our overall health and especially our brain health is growing rapidly. Mayer, et al stated "the discovery and the explosive progress in the characterization of the gut microbiome have initiated a paradigm shift not only in medicine, but also in the basic and clinical domains of neuroscience." in their article "Gut Microbes and the Brain: Paradigm Shift in Neuroscience".(11) Children and adults with Down syndrome are not exempt from this information. They experience a higher rate of c-section births (12), lower rate of breastfeeding (13) and greater exposure to antibiotics.(14) These are the three things that have the greatest impact on the health of an infant's developing microbiome early in life that can impact their health into adulthood.(15)
Although much of this research is new it's imperative that Pediatricians and Family Physicians who are committed to helping all of their patients, including those with special needs, be current on this research. It takes, on average, 17 years for research to translate to policy and clinical practice. (16) We, as a global society, don't have that much time. 17 years is a childhood. The rate of autism is growing rapidly and these children will soon be adults. A shift is greatly needed in the current paradigm of medical practice. This includes everything from the attitudes of physicians to the current structure of our healthcare system that only gives doctors 10 minutes with their patients. I've outlined some steps below that I hope parents and physicians will take seriously. We must each look deeply at our own current attitudes and ability to shift our thinking in order to do what's best for the child. It's not about being right; it's about getting it right for these children and their families. Never stop learning and searching for answers. Many children today whose parents are working with doctors trained in looking for and treating the root cause of symptoms are experiencing significant healing, some even losing their diagnosis of autism.
Steps physicians can take to prevent this from happening:
Tips for parents to prevent medical neglect:
Dr. Sidney Baker summarized it best in "Learning About Autism".
I won't go into great detail about her treatment plan as that's outside the scope of this article. What I will say that I did was to treat her undiagnosed and untreated hypothyroidism, remove her from cow dairy formula and gave the mom some safe and very effective remedies for constipation, among other things. At her follow up appointment two months later I got to meet Mary for what seemed like the first time. She was alert, made eye contact (although infrequently), was able to sit up on her own for extended periods of time and she imitated me making some popping noises with my mouth. This was a huge leap in her development in only two months! We still have a lot of work to do to help Mary heal. Much of that work will be to heal her gut after the assault from dairy formula, Omeprazole, Miralax and antibiotics.
Mary's story is not unique. This happens to hundreds and thousands of children with special needs who experience more visits to the doctor's office than other children. These visits often result in prescriptions that are causing more harm than good, not to mention the lack of addressing the root cause of their symptoms. I recognize Mary's delays as being due to hypothyroidism and severe gastrointestinal dysbiosis NOT her having Down syndrome. Addressing hypothyroidism, gut dysbiosis and malabsorption are the biggest ways that children with Down syndrome and other special needs can be helped. Ignoring that environmental factors like mode of delivery, breastfeeding, diet, early exposure to antibiotics and other drugs that impact the microbiome have an even greater role on their health than that extra copy of chromosome 21 is the greatest medical tragedy that these children experience. Dr. Noel Mueller and his colleagues accurately stated "The infant microbiome plays an essential role in human health and its assembly is determined by maternal-offspring exchanges of microbiota. This process is affected by several practices, including Cesarean section (C-section), perinatal antibiotics, and formula feeding, that have been linked to increased risks of metabolic and immune diseases." in their 2015 review article.(9) In addition, it's been well established that children with autism have a greater prevalence of gastrointestinal problems than their typical peers as outlined in "Gastrointestinal Symptoms in Autism Spectrum Disorder: A Meta-analysis". (10) Many believe, given the strong connection between the health of the gut and the health of the brain, that this may be a major causative factor of autism.
The amount of research connecting the impact that our microbiome has on our overall health and especially our brain health is growing rapidly. Mayer, et al stated "the discovery and the explosive progress in the characterization of the gut microbiome have initiated a paradigm shift not only in medicine, but also in the basic and clinical domains of neuroscience." in their article "Gut Microbes and the Brain: Paradigm Shift in Neuroscience".(11) Children and adults with Down syndrome are not exempt from this information. They experience a higher rate of c-section births (12), lower rate of breastfeeding (13) and greater exposure to antibiotics.(14) These are the three things that have the greatest impact on the health of an infant's developing microbiome early in life that can impact their health into adulthood.(15)
Although much of this research is new it's imperative that Pediatricians and Family Physicians who are committed to helping all of their patients, including those with special needs, be current on this research. It takes, on average, 17 years for research to translate to policy and clinical practice. (16) We, as a global society, don't have that much time. 17 years is a childhood. The rate of autism is growing rapidly and these children will soon be adults. A shift is greatly needed in the current paradigm of medical practice. This includes everything from the attitudes of physicians to the current structure of our healthcare system that only gives doctors 10 minutes with their patients. I've outlined some steps below that I hope parents and physicians will take seriously. We must each look deeply at our own current attitudes and ability to shift our thinking in order to do what's best for the child. It's not about being right; it's about getting it right for these children and their families. Never stop learning and searching for answers. Many children today whose parents are working with doctors trained in looking for and treating the root cause of symptoms are experiencing significant healing, some even losing their diagnosis of autism.
Steps physicians can take to prevent this from happening:
- See the patient as a person first. Recognize that their diagnosis doesn't define them and doesn't always explain every health issue.
- Listen to parents and see them as a partner in helping their child.
- Be open to the idea that there's more that can be done to help children with special needs than medical school has taught most physicians.
- Read up on the impact that gastrointestinal microbial dysbiosis can have on a person's health and cognition. (Brain Maker by Dr. David Perlmutter)
- See the patient holistically and understand that improvements in overall health can lead to improvements in brain health and cognition. (Reversal of cognitive decline: A novel therapeutic program)
- Study the symptoms of hypothyroidism and don't ignore them in any patient, especially those with Down syndrome. (Neonatal hypothyroidism, Hypothyroidism)
- Gain an appreciation for epigenetics and understand that our health is not dictated by our genes alone.
Tips for parents to prevent medical neglect:
- Don't ever let any physician use the excuse "that's just Down syndrome" (or whatever diagnosis your child has).
- If your physician isn't willing to do the first three steps above then find another physician who is willing to do so.
- Understand that your child's potential is much greater than has ever been thought possible and if your child doesn't seem to be reaching their fullest potential there could be an underlying medical reason outside of the extra chromosome or diagnosis. Here's an example of someone who's breaking stereotypes: All lives matter | Karen Gaffney | TEDxPortland
Dr. Sidney Baker summarized it best in "Learning About Autism".
Parents frequently tell me that their kindly pediatrician has responded to their plea for direction with the question, “So you think you can find a cure for autism?” “No,” they say through angry tears, “we just want to help our child.” (17)
No one is questioning the intentions of physicians. Naturally, their intention when writing a prescription is to help their patient. Most physicians truly want to help their patients. In order to do so, however, some changes are needed in the way conventional physicians see their patients with special needs. I highly recommend that all physicians who have patients with autism and Down syndrome read Dr. Baker's article I cited here. The attitude that he conveys applies not only to children with autism but to children with Down syndrome as well. Physician's should ask themselves, "Am I doing EVERYTHING possible to help my patient?". I ask myself this same question all the time.
I encourage parents to briefly share your child's story in the comments below if you've experienced this so that others can see how common this truly is.
I encourage parents to briefly share your child's story in the comments below if you've experienced this so that others can see how common this truly is.
- Konrad TR, Link CL, Shackelton RJ, et al. It’s about time: Physicians’ perceptions of time constraints in primary care medical practice in three national healthcare systems. Medical care. 2010;48(2):95-100.
- Dugdale DC, Epstein R, Pantilat SZ. Time and the Patient–Physician Relationship. Journal of General Internal Medicine. 1999;14(Suppl 1):S34-S40. doi:10.1046/j.1525-1497.1999.00263.x.
- Brian G. Skotko, Susan P. Levine, Eric A. Macklin, Richard D. Goldstein. Family perspectives about Down syndrome.American Journal of Medical Genetics Part A, 2015
- Leung AKC, Sauve RS. Breast is best for babies. Journal of the National Medical Association. 2005;97(7):1010-1019.
- Salvatore S, Vandenplas Y. Gastroesophageal reflux and cow milk allergy: is there a link? Pediatrics. 2002 Nov;110(5):972-84
- Farahmand F, Najafi M, Ataee P, Modarresi V, Shahraki T, Rezaei N. Cow’s Milk Allergy among Children with Gastroesophageal Reflux Disease. Gut and Liver. 2011;5(3):298-301.
- Roušar T., Pařík P., Kučera O., Bartoš M., Cervinková Z. Glutathione reductase is inhibited by acetaminophen-glutathione conjugate in vitro. Physiological Research. 2009;58:239–246.
- http://www.fda.gov/Drugs/DrugSafety/DrugSafetyNewsletter/ucm190244.htm
- Mueller NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG. The infant microbiome development: mom matters. Trends in molecular medicine. 2015;21(2):109-117.
- McElhanon BO, McCracken C, Karpen S, Sharp WG. Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics. 2014;133:872–83.
- Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K. Gut Microbes and the Brain: Paradigm Shift in Neuroscience. The Journal of Neuroscience. 2014;34(46):15490-15496.
- Faro R, Santolaya-Forgas J, Oyelese Y, Di Stefano V, Canterino J, Ananth CV. Cesarean delivery rates in Down syndrome pregnancies. . J Neonatal Perinatal Med. 2013;6(2):109-15.
- Pisacane A1, Toscano E, Pirri I, Continisio P, Andria G, Zoli B, Strisciuglio P, Concolino D, Piccione M, Lo Giudice C, Vicari S. Down syndrome and breastfeeding. Acta Paediatr. 2003 Dec;92(12):1479-81.
- Murdoch JC. Comparison of the care of children with Down’s syndrome with the care of matched controls. The Journal of the Royal College of General Practitioners. 1984;34(261):205-209.
- Neu J, Rushing J. Cesarean versus Vaginal Delivery: Long term infant outcomes and the Hygiene Hypothesis. Clinics in perinatology. 2011;38(2):321-331. doi:10.1016/j.clp.2011.03.008.
- Hanney SR, Castle-Clarke S, Grant J, et al. How long does biomedical research take? Studying the time taken between biomedical and health research and its translation into products, policy, and practice. Health Research Policy and Systems. 2015;13:1.
- Baker SM. Learning About Autism. Global Advances in Health and Medicine. 2013;2(6):38-46.




 RSS Feed
RSS Feed