| Down syndrome, as many who are reading this know, is caused by an extra copy of chromosome 21. The overexpression of the enzymes coded for from genes on this chromosome cause imbalances in methylation and oxidative stress within the body (1, 2, 3). Imbalances of these two processes are implicated in the neurodegeneration and cognitive impairment associated with Down syndrome. Addressing these imbalances through the use of diet, vitamins and supplements can make a big impact on cognition and development for a child with Down syndrome. |
Children and adults with Down syndrome experience other health conditions that cause cognitive impairment like hypothyroidism, histamine intolerance, sleep apnea, gut dysbiosis and malabsorption, autoimmune disease, impaired liver detoxification and more. These are not always a direct effect of the extra chromosome and need to be addressed in a way that avoids simply blaming them on the extra chromosome.
It's been my experience after helping over a thousand children with Down syndrome that not all children respond well on these protocols. Some even regress or parents notice an improvement in development when they take them off. Some do well and some don't. Many patients come to our practice already taking supplements from one of these protocols and are still struggling with hypothyroidism, delayed development, severe digestion issues, neuropathies secondary to vitamin deficiencies and more. The vitamins and nutrients in these protocols may not even be absorbed if the patient is experiencing significant gut dysbiosis and malabsorption issues. Only an experienced practitioner with training in functional medicine can determine if this is occurring or not.
The use of organic acid testing through a urine sample can help practitioners and parents understand their child's unique biochemistry. Organic acid testing is only one example of functional medical testing that can help a physician uncover the true underlying cause of disease. Other testing options include stool analysis, heavy metal testing, salivary cortisol testing and blood tests for iron, zinc, copper, B12, histamine and thyroid hormones.
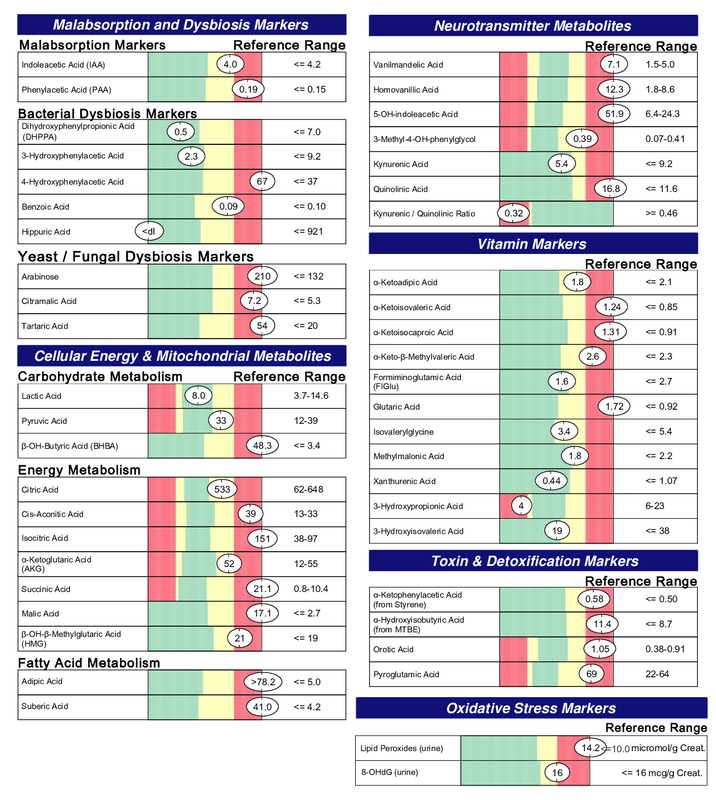
Below is an example of a Metabolomix. It's a urine organic acid test from Genova Diagnostics. This was run for a 14 month old child with Down syndrome on no supplements (Image 1). This child was receiving thyroid hormone to address hypothyroidism, which is one of the biggest causes of slow gut motility in children with Down syndrome, but was still struggling with his health. These are typical results that I see in my practice. I will explain these results in very simple terms to help readers understand the overall information we can get from this kind of testing. There is a lot of detail I and other functional medical practitioners gain from doing organic acid testing that is outside the scope of this blog post.
- Elevated malabsorption markers that are indicative of small intestinal bacterial and yeast overgrowth.
- Elevated intermediates of the citric acid cycle indicating poorly functioning mitochondria.
- Elevated markers of fatty acid metabolism tell us that his mitochondria are not using them as fuel as they should be.
- Elevated neurotransmitter markers tell us that his body is not properly metabolizing these neurotransmitters. Elevated quinolinic acid seen in the neurotransmitter section is an indication of inflammation in the central nervous system (brain).
- Elevations in vitamin marker metabolites indicate a need for extra B1, B2 and B3.
- Toxin and detoxfication markers are elevated revealing poorly functioning detox pathways. These do not mean that he is being overly exposed to these toxins. These toxins are normally processed in the liver and excreted through the stool. These are markers in his urine telling us that they are in his blood and not being excreted properly by the liver and digestive system. They can also be elevated secondary to his need for methylation support and glutathione.
- Lastly, his elevated markers of oxidative stress can be a result of the extra chromosome but can also be a result of his need for vitamin B1, B2, B3 and mitochondria function.
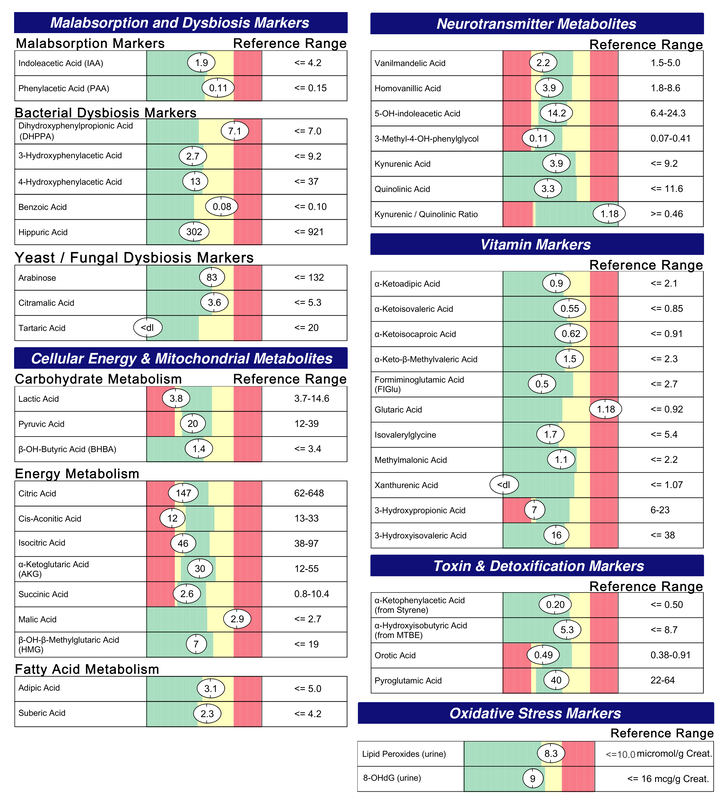
- Normalized malabsorption and dysbiosis markers (no more bacterial or yeast overgrowth)
- Normalized mitochondria function
- Normalized neurotransmitter metabolites
- Normalized quinolinic acid indicating a reduction in central nervous system inflammation
- Normalized vitamin markers, except for glutaric acid which indicates need for B2. This was addressed with the addition of riboflavin to his plan.
- Normalized detoxification
- Normalized in markers for oxidative stress
It should be noted that these results are not typical. It often takes many months of adjusting supplements and diet and repeat running of this test to get these results. However, this child is an example of what's possible after only 3 months. One of the main reasons this child did so well was because we focused on healing the gut and withheld all other supplements that could potentially feed the yeast and bacteria in his gut. As a result of this treatment his health, development and cognition all showed great improvement.
What I've learned from running this test and others like it on many children with Down syndrome is this. All children with Down syndrome experience different imbalances in biochemical processes and organ function. Some actually experience very few imbalances. This results in a different approach that is needed for each child. Their health issues that contribute to poor cognitive function are not simply due to an extra copy of chromosome 21. The fact that they have an extra copy of this chromosome cannot be ignored, however. Research exists supporting improved cognition in the Down syndrome model (mice and humans) when agents are used that block key enzymes coded for on chromosome 21 (8).
The bottom line is supporting the health and cognition of our loved ones with Down syndrome requires a multi-level approach that goes beyond supplementing with a protocol. We cannot simply inhibit the extra chromosome, block malfunctioning neurotransmitter receptors or give vitamins that have been deemed beneficial for every child with Down syndrome. They must be treated as individuals.
This may be disheartening to some parents who do not have access to a functional medical doctor that can run, interpret and properly treat based on more advanced testing like the Metabolomix test. My goal is to change that.
Functional medicine addresses the underlying cause of disease using a systems-oriented approach. The field is growing as more and more physicians, patients and parents become frustrated with the ineffectiveness of pharmaceuticals that simply address symptoms and not the underlying cause of disease. Making functional medical doctors aware that they can help children and adults with Down syndrome is key. Customized medicine is the future of healthcare and children with Down syndrome are not and should not be excluded from the benefits of this deeply healing form of medicine.
- Pogribna M, Melnyk S, Pogribny I, Chango A, Yi P, James SJ. Homocysteine Metabolism in Children with Down Syndrome: In Vitro Modulation. American Journal of Human Genetics. 2001;69(1):88-95.
- Jovanovic SV, Clements D, MacLeod K. Biomarkers of oxidative stress are significantly elevated in Down syndrome. Free Rad Biol Med. 1998;25:1044–8
- Obeid R., Hartmuth K., Herrmann W., et al. Blood biomarkers of methylation in Down syndrome and metabolic simulations using a mathematical model. Molecular Nutrition and Food Research.2012;56(10):1582–1589. doi: 10.1002/mnfr.201200162.
- Mendioroz M, Do C, Jiang X, et al. Trans effects of chromosome aneuploidies on DNA methylation patterns in human Down syndrome and mouse models.Genome Biology. 2015;16:263.
- Strydom A, Dickinson MJ, Shende S, Pratico D, Walker Z (2009) Oxidative stress and cognitive ability in adults with Down syndrome. Prog Neuropsychopharmacol Biol Psychiatry. 1 33(1): 76–80
- Karmiloff-Smith A, Al-Janabi T, D'Souza H, et al. The importance of understanding individual differences in Down syndrome. F1000Res. 2016;5:F1000 Faculty Rev-389. Published 2016 Mar 23.
- Lana-Elola E, Watson-Scales SD, Fisher EMC, Tybulewicz VLJ. Down syndrome: searching for the genetic culprits. Disease Models & Mechanisms. 2011;4(5):586-595. doi:10.1242/dmm.008078.
- Torre R, Sola S, Pons M, et al. Epigallocatechin-3-gallate, a DYRK1A inhibitor, rescues cognitive deficits in Down syndrome mouse models and in humans. Mol Nutr Food Res. 2014;58(2):278–288.



 RSS Feed
RSS Feed