Introduction
| There's a lot of talk online about gut health these days. It's for good reason and I'm very encouraged to see so many parents learning about the importance of gut health when working to optimize their child's overall health. If I had to pick the most important area of health that I focus on to help my patients it would definitely be optimizing gastrointestinal health and a big part of that is to support gastrointestinal motility. The health of our whole body depends on the health of our gut. A healthy gut involves many factors including an intact epithelial lining, healthy balance of bacteria and yeast, optimally secreting organs of digestion (stomach, liver/gallbladder, pancreas) and definitely optimal gut motility. I'll explain the consequences of slow gut motility, signs and symptoms of slow gut motility, major physiological factors impacting gut motility, and treatments that can help improve it. |
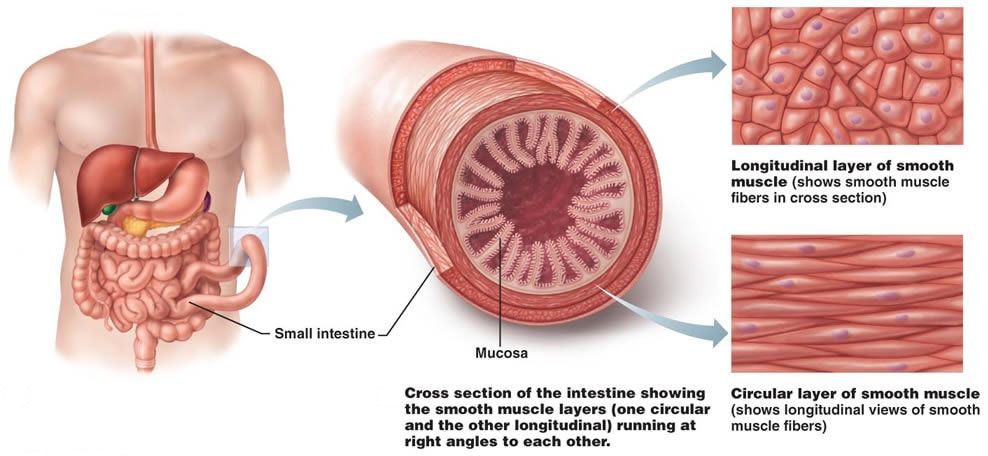
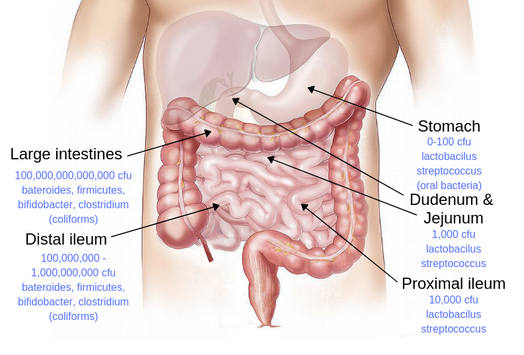
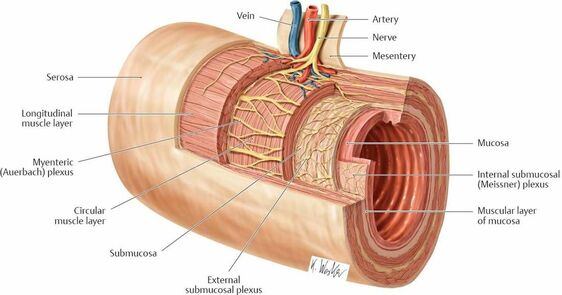
Let's start by briefly reviewing gastrointestinal anatomy. Basically the gut largely consists of smooth muscle. It is essentially a muscular organ (Image 1). The interior lining of these muscles, the mucosa, is where the very important task of secretion and absorption occurs.
| Smooth muscle contractions are not linear like those of skeletal muscles. They occur in all directions which results in a concentric narrowing of the gut lumen. A coordinated series of contraction and relaxation happen in waves along the entire length of the GI tract resulting in peristalsis and movement of food and stool within the lumen. (Image 2) |
Consequences of Gut Motility Issues
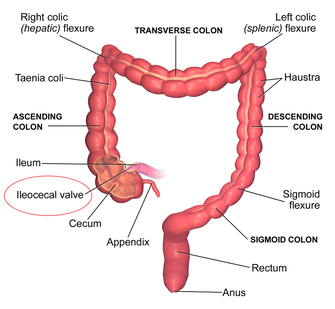
| The sphincter between the large intestines and the small intestines is called the ileocecal valve (Image 5) or the ileocolonic sphincter (ICS). It serves as a very important mechanical barrier between these two distinct segments of the gut. A retrograde (backward) flow of contents from the large intestines creates a higher concentration of bacteria built up in the ileum which defines small intestinal bacterial overgrowth (SIBO). |
Signs and Symptoms
| The symptoms of decreased gut motility include a lot more than just constipation. To add to that, constipation is a lot more than just decreased bowel movement frequency. Meaning, a child can experience a bowel movement every day but still have slow gut motility that is impacting absorption in their small intestines. The following is a list of symptoms seen in children with slow gut motility:
|
Enteric Nervous System
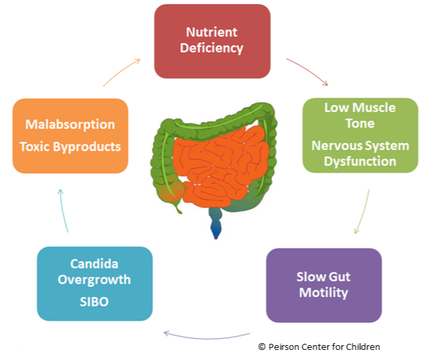
You can see how SIBO, which can cause a vitamin B1 and B3 deficiency, among other things, can further impair gut motility by negatively impacting ACh synthesis and vagus nerve function. It is the perfect example of a vicious cycle.
Mitochondria
Nutrients that support mitochondrial function and therefore support gut motility include:
- Carnitine
- CoQ10
- B Vitamins
- Ribose
- T3/T2 hormone
- Creatine
Of those compounds listed above the one most noted for it's effects on gut motility is carnitine. Researchers in Japan studied carnitine levels in 27 patients with severe motor and intellectual disabilities. They found that the severity of their constipation correlated significantly with the levels of carnitine found in their blood samples. They supplemented carnitine in those who were deficient and saw a significant reduction in their constipation. (Murata, et al 2014) This has also been the experience of many parents using carnitine to help their child with slow gut motility.
For a more thorough look at mitochondrial dysfunction, how to test for it and how to treat it you can read Mitochondria - Why They're Important and What They Need to Function
The video below shows how muscles use ATP to contract or essentially shorten.
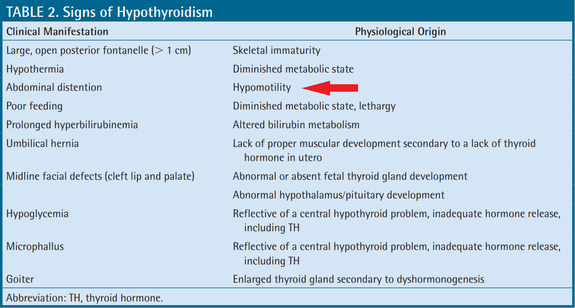
Thyroid
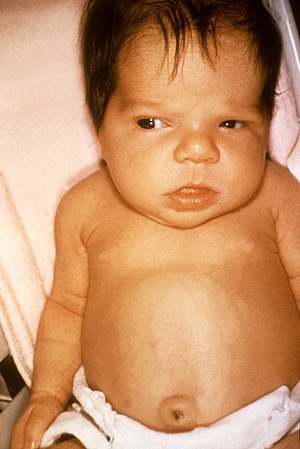
| Thyroid hormone acts on all organs of the body, the gut is no exception. Delayed gut motility is a hallmark of hypothyroidism. Hyperthyroidism can have equally detrimental effects on gastrointestinal health and function. Hypothyroidism is marked by an accumulation of glycosaminoglycans, like hyaluronic acid, within soft tissue of the body creating edema and swelling. This substance is essential for healthy joints as it helps to lubricate and cushion them. It becomes a problem when it builds up in areas beyond healthy levels. In hypothyroidism it mostly builds up under the skin and in muscle, including the muscles of the gut. The deposition of this substance within muscles hinders it's ability to contract properly. Many people with hypothyroidism experience diffuse skeletal muscle pain due to this aspect of their hypothyroidism. In adults, this is not only seen as symptoms of muscle pain it can also be seen visibly as edema under the skin particularly in the lower extremities and the face. In children it presents more often as edema in the abdomen and face as seen in Image 8. |
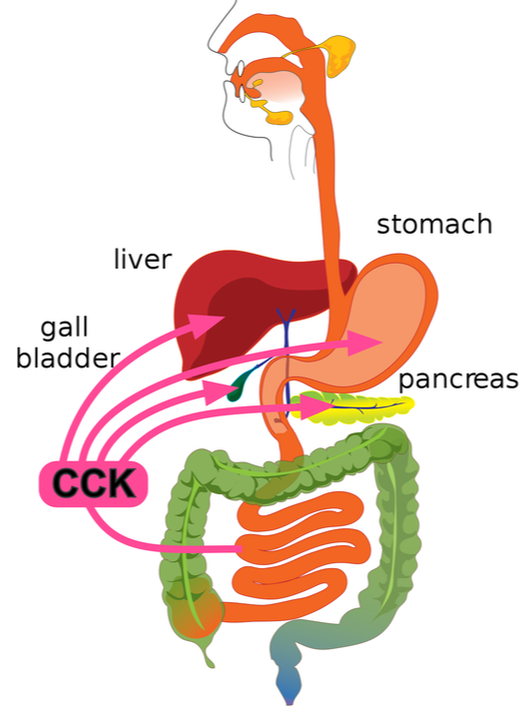
Cholecystokinin
| Cholecystokinin (CCK) is a hormone secreted from enteroendocrine cells in the first segment of the small intestines (duodenum), but are found throughout the the small intestines as well. It's released in response to the presence of fat and protein in the digestive tract when eating. It's also triggered by HCl (hydrochloric acid) secretion from the stomach. CCK facilitates digestion in several different ways. (Image 10) It triggers release of bile from the gallbladder and digestive enzymes from the pancreas. CCK also is found within the brain and other parts of the central nervous system. In fact, CCK "is one of the most the abundant and widely distributed neuropeptides in the brain." (Lee and Soltesz 2011) CCK acts as a neurotransmitter within the brain and signals satiety (feeling of fullness) and sleepiness. It's action on the nervous system is not only found within the central nervous system, it also acts on the vagus nerve and the enteric nervous system. |
- reduced satiety
- trouble sleeping
- gallstones/gallbladder issues
- low pancreatic elastase on stool analysis
- obesity
- slow gut motility
- Increase fats in the diet, especially olive oil
- Protein with every meal
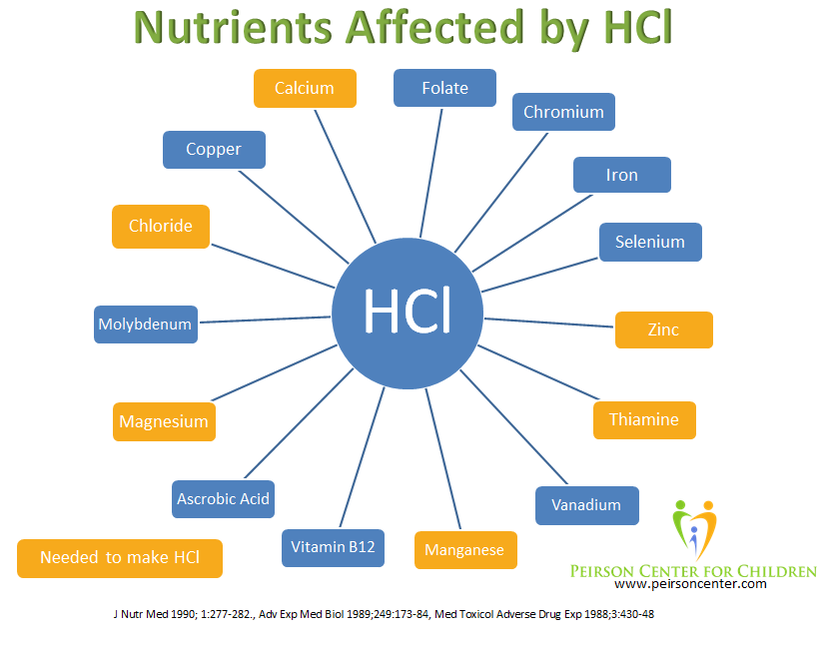
- Optimize stomach acid (HCl) production (Image 11)
- Include beans in the diet (Bourdon et al 2001)
Be careful with beans in the diet for those with small intestinal bacterial overgrowth (SIBO) as the fiber and sugars in beans can cause increased gas and bloating. Focus on olive oil and protein. The amount of protein an average child needs is approximately half their weight (lbs) in grams. So, a 40 pound child will only need approximately 20 grams of protein per day. You don't want to give too much protein to a child with SIBO either as the excess levels of bacteria in the gut can produce ammonia from the protein.
Serotonin
5-HT is made from tryptophan, an essential amino acid. Essential amino acids are those that our bodies can't make and must be obtained from the diet. About 90% of tryptophan is used to make nicotinamide (vitamin B3), a cofactor needed for energy production within the body. (Lugo-Huitrón, et al 2013) The other 10% is used to make 5-HT in a process that is dependent on vitamin B6. The availability of tryptophan can therefore influence the production of 5-HT in the body. To learn more about how tryptophan is used to make both nicodtinamide and 5-HT watch the video below.
One very important factor that can lead to a decrease level of 5-HT within the gut is inflammation. A disruption in the balance if bacteria and yeast within the gastrointestinal microbiome is a major cause of inflammation within the gut. (Nishida, et al 2018) Researchers in the Netherlands have stated "...in a state of inflammation, not only high levels of proinflammatory cytokines are produced but also altered levels of neurotransmitters, such as serotonin, a derivative of tryptophan metabolism, are detected in the gut." (Waclawiková and Aidy 2018)
So, we have another vicious cycle: disturbed microbiome → inflammation → low serotonin → slow gut motility → disturbed microbiome → etc.
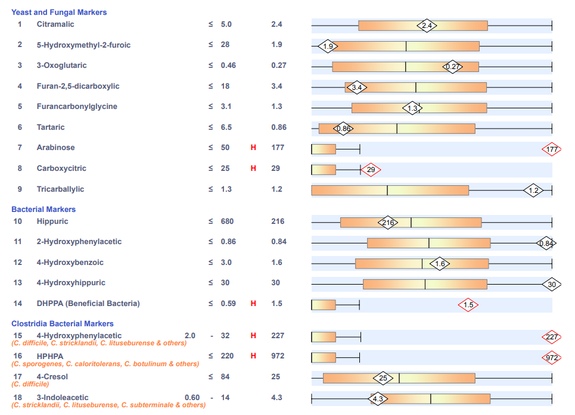
Testing
A simple, at home test involves the use of activated charcoal. This can be obtained cheaply in capsule form. Activated charcoal is used often in research to test gastrointestinal transit in animal studies, typically in mice. Activated charcoal is often used at home and in hospital settings to absorb orally ingested poisons. It's a good thing to have on hand in any home with small children for this purpose. It's not absorbed by the body and remains in the gut. Due to it's dark color it can be easily detected in stool. For this reason, it makes for a great tool to measure bowel transit time. Capsules can be opened or swallowed whole depending on the age and skill of the child. The number of capsules used will depend on the age of the child. Adults can use 4-6 capsules, young children can take 2-4 capsules and toddlers can take 2 capsules. Capsules are given all at once right after a bowel movement. Activated charcoal has almost not flavor, but a slightly gritty texture. It can be mixed in juice to help young children get it down. It will make the juice pitch black so consider putting it in an opaque cup so the child isn't put off by the color. Note the date and time the charcoal was given. Inspect every bowel movement under bright light after the charcoal is given, looking for signs of black in the stool. Write down the date and time the charcoal is first seen. This is the time it took for the charcoal to pass through the digestive tract. Calculate the number of hours between when capsules were swallowed and when the first sign of black color appeared in the stool. Continue to examine every stool, and note the time and date when the black color has completely disappeared. An optimal bowel transit time for children and adults is 18-24 hours. Anything less than 18 hours is considered a fast transit time, more than 24 hours is a sign of slow gut motility.
| An x-ray of the abdomen can be used to detect gas, fluid and stool within the gut. The x-ray usually ordered for this purpose is called a KUB. It carries this name because it is also used to view the kidneys, ureters, and bladder. X-rays typically are used to look at bony structures and calcifications but can also be used to see gas and soft tissue. Image 8 is an example of what might be seen in a child who is experiencing abdominal pain or discomfort from constipation. An organic acid test is another test that can help give clues to gut motility and is ordered by a physician. This is the best test to use to assess makers of digestion, malabsorption, mitochondrial function, fatty acid metabolism, vitamin deficiencies and oxidative stress. Elevated levels of yeast activity together with elevated levels of bacterial activity are strong indicators of gut motility issues. |
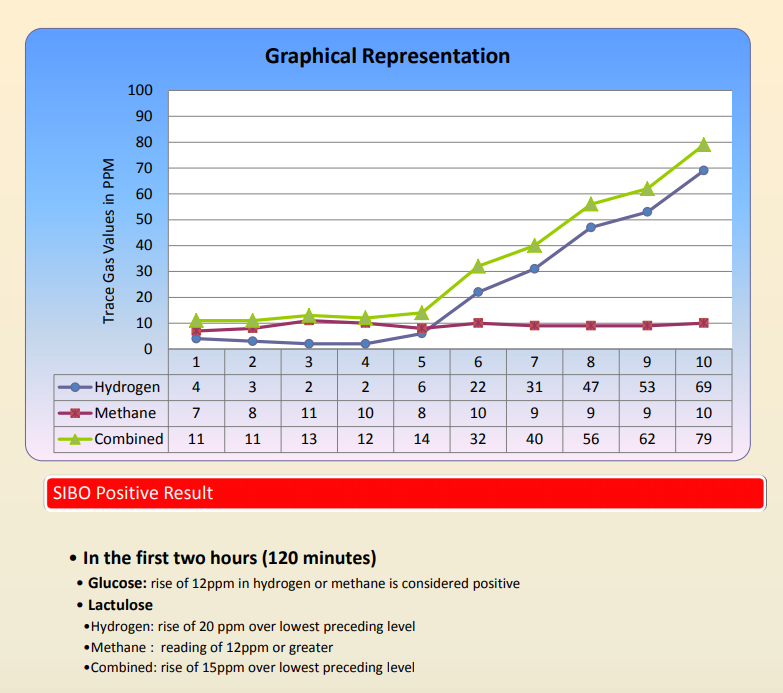
| A discussion of tests for gut motility cannot go without mentioning the hydrogen breath test. This test can be difficult for most children to do and only needs to be done when other tests are inconclusive. It involves the oral ingestion of a solution of either lactulose of glucose. Both of these sugars increase fermentation by anaerobic bacteria in the colon resulting in an excess production of hydrogen and methane gases. As explained earlier these anaerobic bacteria can also be present in the small intestine in SIBO, increasing the production of hydrogen and/or methane. Some production of these gases is normal but elevated levels, as seen in Image 10 are an indication of SIBO. |
Treatment
The main underlying causes to address when considering treatment include:
- ACh synthesis
- Micronutrient deficiencies
- Methylation issues (needed for choline synthesis)
- Nervous system function
- Mitochondrial function
- Thyroid hormone function
- HCl, gallbladder and pancreatic function
- Inflammation
- Diet
Herbs
Herbs that improve gut motility can be very helpful to alleviate the symptoms until the root cause can be uncovered and addressed. They can also be helpful to break the vicious cycle of malabsorption secondary to elevated levels of yeast and bacteria. Below are some of my favorite and most effective herbs to help improve gut motility.
Iberis Amara (Candytuft) is the main ingredient of Iberogast. This is a popular herbal formula used in Europe but can also be found in the US. Its often recommended for those with SIBO due to it's ability to increase gut motility. Other ingredients in Iberogast include Mentha piperita L., Matricaria chamomilla, Glycyrrhiza glabra, Angelica archangelica, Angelica archangelica, Silybum marianum, Melissa officinalis and Melissa officinalis. These herbs work synergistically to help optimize digestion and gut motility. German researchers found Iberis amara extract created "clear differences" in the symptoms of IBS over placebo in a multicenter, prospective, double-blind, randomized parallel group comparison. (Reichling and Saller 2002) Ten years later it was stated, "Double-blind and randomized studies versus placebo or active control found statistically significant effects of STW 5 (Iberogast) on patients’ symptoms with a comparable efficacy to a standard prokinetic." (Ottillinger, et al 2012). You can find prescribing information on the package insert here.
Bacopa monnieri (Brahmi) is an Ayurvedic herb that has been used for centuries in children. Adverse effects are rarely reported, but one side effect that it can have is increased intestinal motility. It has acetylcholinesterase inhibition properties, which means it increases levels of acetylcholine within the body. This ultimately results in improved cognition and improved gut motility. (Aguiar and Borowski 2013)
Aloe vera juice is a common, safe and effective remedy for constipation. It helps alleviate gut permeability due to it's anti-inflammatory and soothing properties. One of the key components of aloe is barbaloin which is metabolized to aloe-emodine-9-anthrone by intestinal bacteria. Aloe-emodine-9-anthrone increases intestinal motility. (Hong, et al 2018)
Foeniculum vulgare (Fennel seed) is more commonly know for it's effects on relieving gas. This makes it a very popular and effective remedy for helping babies with colic. Fennel also has been shown to stimulate the smooth muscles of the small intestines. (Alexandrovich, et al 2003) It can be given as a tea or fennel essential oil that is labeled for oral consumption can be used in very small doses.
Osmotic diuretics
Osmotic diuretics do nothing to optimize gut motility and only act as bandaids to the problem by making stool softer. The most commonly prescribed pharmaceutical agent prescribed to those with slow gut motility and constipation is polyethylene glycol - 3350, known as MiraLAX in the US or Movicol and Macrogol in other countries. It works by drawing water into the large intestine resulting in softer stool that is easier to pass. It does not improve gut motility and definitely doesn't address the root cause of slow gut motility. Other, safer and more natural osmotic diuretics exist and include magnesium oxide and high dose vitamin C. We highly encourage our patients to avoid Miralax given the controversy over it's safety. (Welch 2017) Miralax is not labeled for use in those under 17 years of age and is only to be used for occasional, short term constipation. The label clearly states “use no more than 7 days” because it should not be used to address chronic constipation. (Image 11) My biggest concern with it being used for chronic constipation is it addresses the symptom of constipation yet leaves the underlying cause unaddressed. Several of these underlying causes mentioned above can result in permanent neurological damage to very young children.
Probiotics should be considered carefully when treating children with gastrointestinal motility issues. In some they can improve gut motility and in others they can aggravate constipation and symptoms of SIBO. Recall that SIBO is an increased level of bacteria in the small intestines, therefore, probiotics can aggravate it. Taking a probiotic with the right strains is extremely important as well.
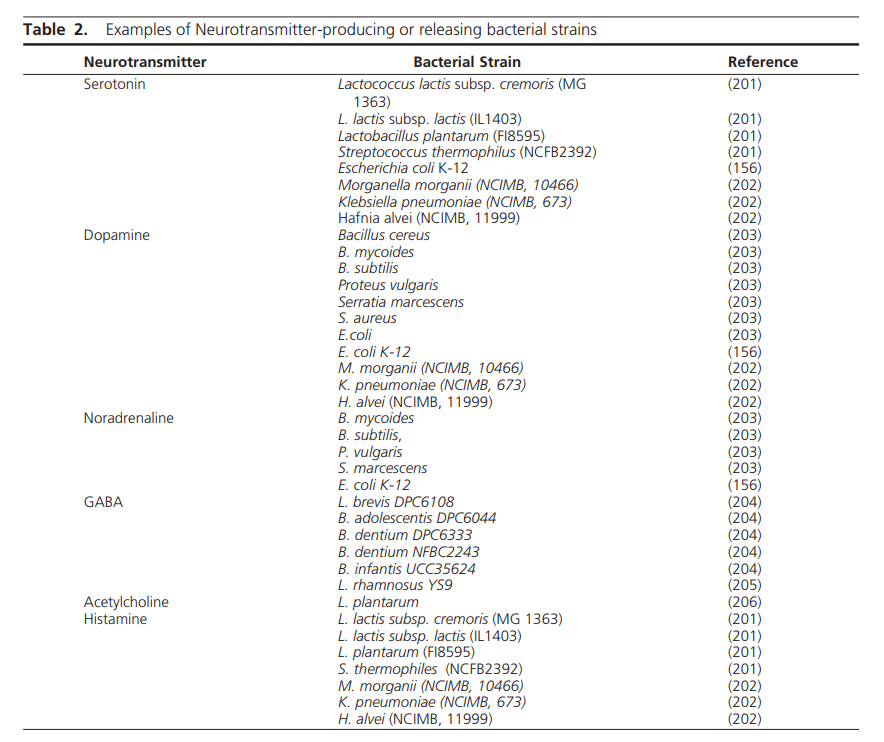
Bacteria in the gastrointestinal microbiome serve many roles for it's human host. They are involved in nutrient metabolism, vitamin synthesis, short chain fatty acid synthesis that supports the lining of the gut, phenol metabolism, immune system homeostasis and xenobiotic and drug metabolism. (Jandhyala, et al 2015) In 2014 a team of scientist at the Alimentary Pharmabiotic Centre in Ireland reported that neurotransmitter synthesis can also be added to that list. (Clarke, et al 2014) The term endocrine is defined as "Pertaining to hormones and the glands that make and secrete them into the bloodstream through which they travel to affect distant organs" (medicinenet.com) Clarke and his team argue that the gut microbiome acts as an endocrine organ because of it's ability to secrete compounds that act on distal organs such as the brain. They include a list of bacterial strains and the neurotransmitters that are produced by these specific strains seen in Image 12. Several of these strains listed are considered pathogenic like Klebsiella penumoniae, Hafnia alvei and Morganella morganii. The presence of these strains within the gut microbiome can result in increased gut motility seen as diarrhea potentially due to their production of serotonin and histamine which can increase gut motility. (Fabisiak, et al 2017)
Clinical evidence reveals the eradication of pathogenic bacteria and yeast along with the replenishment of beneficial bacteria within the gut often results in an optimization of gut motility, nutrient absorption, neurotransmitter balance, improvements in mood and behavior, immune system function, cognition and overall health of the host. This is supported by research and statements from experts such as, "The gut microbiome affects virtually all aspects of human health." (Mohajer, et al 2018)
A comprehensive stool analysis that includes markers like calprotectin, esosinophil protein X, secretory IgA levels, short chain fatty acids, fecal fats, along with the presence of commensal bacteria strains and pathogenic bacteria, yeast and parasites can aide in guiding an appropriate program aimed at improving the gut microbiome. This task is often not a simple one and in some cases can take years of optimizing diet, supplements, antimicrobials, probiotics and herbal prokinetics. The amount of time and effort it can take to correct gut microbiome imbalance can depend on how extensive the initial cause of the imbalance was, such as number of rounds of oral antibiotics or years of proton pump inhibitor use. The presence of biofilm can slow the process as well if not properly addressed. We often tell patients, "This isn't a one and done process". The patients who we see the best results with are those who are able to run functional medical testing like organic acid and comprehensive stool analysis as early as possible and are able to repeat testing at regular intervals (every 3-6 months) to assess the effectiveness of the current treatment program and make necessary adjustments.
Conclusion
The lumen of the gut can be compared to a river. Environmental biologists know very well that the flow of a river dictates the diversity and health of the river. It's been stated, "A river's flow is its heartbeat. Because we have dammed so many rivers and lakes, our freshwater ecosystems are losing species and habitats faster than any other type of ecosystem." (Internationalrivers.org) If the river is slowed and becomes stagnant algae and microbes will grow at a rate that is faster than the river moves them along. This will create an imbalance in the ecosystem of that river that chokes out other life, ultimately creating an unhealthy river.






 RSS Feed
RSS Feed