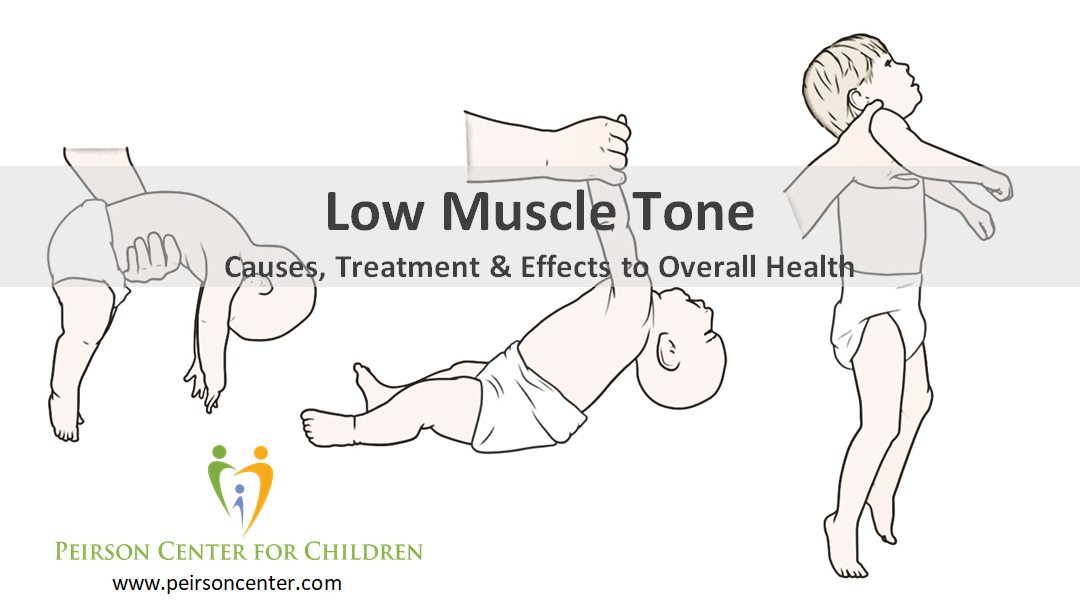
- Head lag
- Fatigues quickly
- Poor posture
- Increased flexibility, increasing susceptibility to injuries
- Poor persistence to gross motor tasks
- Lack appropriate body awareness feedback
- Avoids chewy foods
- Feeding difficulties
- Preference to engage in sedentary activities
An example of an infant with low muscle tone is seen in the video below. (This video may be difficult to watch but this exam is being conducted by a very experienced physician. We don't recommend that you attempt a head lag test on your own child with low muscle tone.)
- Hypothyroidism
- Mitochondrial dysfunction
- Methylation issues
- Thiamine (B1) deficiency
- Other B vitamin deficiencies
- Carnitine deficiency
- Creatine deficiency
- TSH, free T4, free T3, reverse T3
- homocysteine
- acylcarnitine profile
- amino acids (plasma and/or urine)
- organic acids in urine
- creatinine
This is not an exhaustive list as there are many other labs to consider depending on the history and presentation of the patient. Other labs to consider are vitamin D, ferritin, CBC and histamine. For more information about urinary organic acid testing please see our web page devoted to information about this very informative and important testing method: Organic Acid Testing. Naturally, lab results will guide appropriate treatment.
Physicians should be aware of all causes of low muscle tone and seek out appropriate testing in order to best treat it. Often children are referred for physical therapy and orthotic braces alone and no biochemical cause is pursued, especially when the child has a known genetic condition. While therapy and orthotics are often helpful they do not address the underlying cause of the low muscle tone. When any one of the causes listed above is missed this can greatly impact brain development, cognition and the overall health of the child.



 RSS Feed
RSS Feed