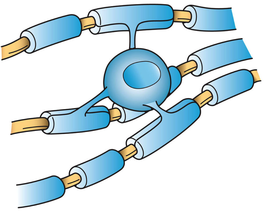
| The amount of white matter we have in our brains is vital to proper brain function. The substance that makes up white matter is a fatty protein called myelin. The fat component is what gives myelin it's white appearance. In the brain this substance is created by specialized cells called oligodendrocytes (image 1). They have multiple projections or arms that wrap around nerve axons to insulate them. The presence of this insulating layer is essential for nerve conduction. Normally a nerve impulse travels down an axon in a wave. In the prescence of myelin sheaths the impulse jumps and moves exponentially faster. |
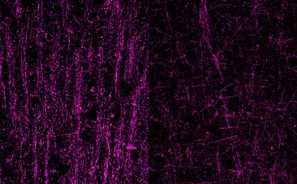
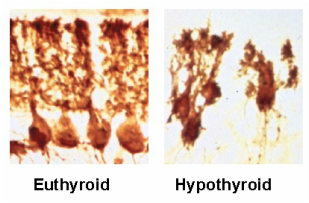
| Without this myelin layer nerves don't communicate with one another properly. Image 2 shows an unmyelinated neuron on the left and a myelinated neuron on the right. It depicts how more rapidly an impulse moves when the neuron is myelinated. White matter is most dense in the interior of the brain as seen in Image 3. The gray matter on the cortex or outer shell of the brain is darker because that's were the cell bodies of most neurons exist. The nucleus and other cell organelles are found in the cell body, giving the darker appearnace. In addition, cell bodies are not myelinated. The cell bodies of the neurons in Image 2 are at the top. |
| A new study, published this week in Neuron, reveals changes in early development and differentiation of these oligodendrocytes that make myelin. They also found actual hypomyelination if Ts65Dn mice (genetically modified to model Down syndrome in humans). Many researchers speculate that changes in brain development in utero are the root of cognition changes later in life for individuals with T21. |
- Fatigue
- Flu-like symptoms
- Depression and mood changes
- Gastrointestinal problems (6)
There's support for other means of optimizing myelination than just ensuring proper thyroid hormone function. B12 and folate are critical for early brain development and myelination formation in utero. (8) Most importantly, however, is iron. Todrich, et all have stated, "The importance of iron in myelin production has been demonstrated by studies showing that decreased availability of iron in the diet is associated with hypomyelination. " (9) Radlowski and Johnson stated, "...the need and usage of iron by oligodendrocytes does not end during the perinatal period and that the adult brain still requires adequate iron." (10) Iron levels are commonly low in children with Down sydrome. (11, 12)




 RSS Feed
RSS Feed