- Exacerbation of aging
- Degeneration of anatomical pathways
- Exposure to aluminium
- APOE gene
- Mitochondria dysfunction
- A compromised blood brain barrier
- Immune system dysfunction
- Infectious agents
Armstrong further explained that AD is multifactorial, which is restated by many other authors:
- Alzheimer Disease, a Multifactorial Disorder Seeking Multi-therapies - Igbal 2010
- The multifactorial nature of Alzheimer's disease for developing potential therapeutics.- Carreiras 2013
- The Complex and Multifactorial Nature of Alzheimer’s Disease -Alkadhi 2010
- Toward a multifactorial model of Alzheimer disease - Storandt 2012
I'll review here factors other than amyloid protein and the APP gene that have been proposed as contributing factors to AD and how those same factors are experienced by people with DS. The management and treatment of these factors, many of which are lifestyle related, can greatly reduce the chances of anyone developing AD, even those with DS. Those factors are:
- Low T3 (active thyroid hormone)
- Impaired glucose metabolism
- Thiamine deficiency
- Sleep apnea
- Aluminum
- Mitochondria dysfunction
T3 Hormone
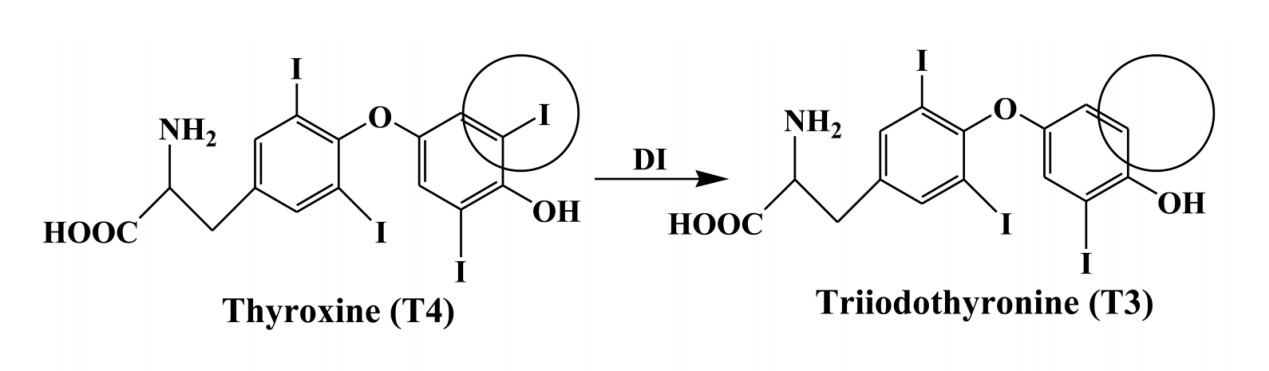
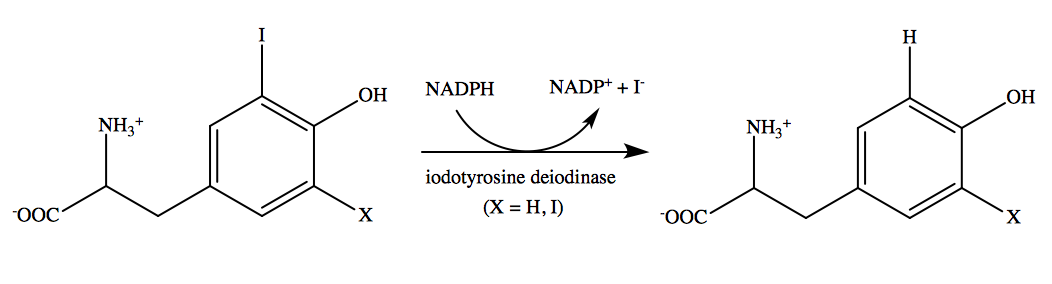
In addition, researchers in Italy found elevated levels of reverse T3 in the cerebral spinal fluid of patients with AD. (Sampaolo 2005). Reverse T3 is a form of T3 hormone created by a different form of deiodinase enzyme that is a sign of aberrant thyroid hormone metabolism. (Biano 2013) Researchers in Japan found that, "Serum rT3 level was a more sensitive parameter than serum T4 or T3 for evaluating thyroid dysfunction." (Shimada 1983) It's also been my experience that reverse T3 levels are elevated in my patients, particularly infants less than one year old as outline here in my research proposal.
Glucose Metabolism
- The Alzheimer's disease-related glucose metabolic brain pattern. (Tuene 2014)
- Brain glucose metabolism in Alzheimer's disease. (Swerdlow 1994)
- Sugar and Alzheimer’s disease: a bittersweet truth (Iadecola 2015)
- Abnormalities of glucose metabolism in Alzheimer's disease. (Hoyer 1991)
- Brain fuel metabolism, aging, and Alzheimer's disease. (Cunnane 2011)
- Abnormal Glucose Metabolism in Alzheimer's Disease: Relation to Autophagy/Mitophagy and Therapeutic Approaches. (Banerjee 2015)
- ...and many others
Researchers at the Imperial College of London stated, "The impaired glucose metabolism in the brain of subjects with AD is a widely recognized early feature of the disease". (Calsolaro 2016)
For a further review of glucose metabolism and the brain I recommend reading "Sugar for the brain: the role of glucose in physiological and pathological brain function".
Thiamine
The enzyme complex pyruvate dehydrogenase (PDHC) is a key step in glucose metabolism. The cofactors for this enzyme are thiamine (B1), riboflavin (B2) and alpha lipoic acid. PDHC activity was found to be reduced in AD and Huntington's disease indicating a deficiency in one or all of these cofactors. (Sorbi, 1983)
A five year study of 76 elderly patients with mild AD being given benfotiamine is currently underway at Cornell University and will be completed in 2019. (National Institute of Aging) Given the positive results seen in previous studies the results are likely to be positive for some of these patients.
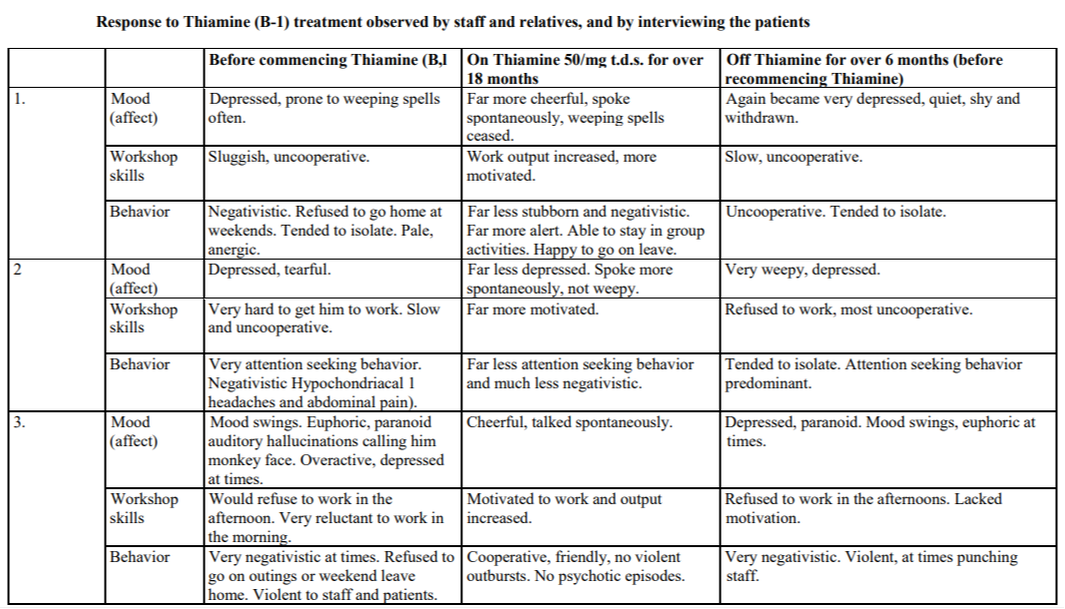
Two published clinical trials exist using thiamine in two different forms in people with DS. The first one was conducted in 1979 and included three adult subjects with DS. While the size of this trial was small the results were significant. Although not clearly stated, the form of thiamine used was likely thiamine HCl or thiamine mononitrate as these are the more common forms used. They gave 50 mg three times a day. The results are recorded in the center column of Table 2 below. (Reading 1979)
Again, my experience with using thiamine is in much younger children, and with benfotiamine as the form. To this day a clinical trial investigating the use of benfotiamine (that is non-toxic) in those with DS has not been conducted. My hope is that it would include young children ages 1-3 years given the sensitive nature of brain development at this age.
Sleep apnea
Our bodies generate energy from glucose in two ways, aerobic respiration (with oxygen) and anaerobic respiration (without oxygen). Aerobic respiration is the preferred form of energy production because it involves the mitochondria and makes a significantly higher amount of energy. In the absence of oxygen pyruvate (made from glucose) cannot enter the mitochondria. Pyruvate is then converted to lactate and mitochondria sit unused. You can watch the video below to learn more about anaerobic and aerobic respiration.
So, in the absence of oxygen the brain can experience elevated levels of lactate, also known as lactic acid. This is the same lactic acid that creates sore muscles after a strenuous workout. A person can feel like they've had a hard workout just from experiencing hypoxia due to obstructive sleep apnea (OSA) at night without the benefits of the strenuous workout. Anyone who as experience with sleep apnea has an increased chance of also experiencing muscle pain. Researchers in Turkey found a "55.4% prevalence of chronic widespread pain in patients with obstructive sleep apnea". (Aytekin 2015) This pain is often due to a build up of lactic acid within muscles.
This same lactic acid can build up in the brain as well and is very toxic to brain cells due to it's acidic nature. In fact, research exists linking elevated lactic acid to amyloid plaques and AD. Researchers at the University of Florida found elevated levels of lactic acid in cerebral spinal fluid of patients with AD. (Xiang 2010) A team in Italy found the same thing in 2015. (Liguori 2015)
The level of hypoxia experienced during OSA varies from patient to patient. Researchers in India measured serum lactate and uric acid levels in patients wit OSA and their conclusion reads, "Both serum UA and lactate were positively correlated with the degree of hypoxia in OSAS. The plasma UA levels in patients with OSAS did not show an overnight rise. However, the plasma lactate levels were higher in the morning. The measurement of serum lactate level was a better marker of oxidative stress among patients with OSAS." (Hira 2012) Earlier in 2009 a research team in Turkey found elevated arterial lactate levels in patients with sleep-related breathing disorders. (Ucar 2009)
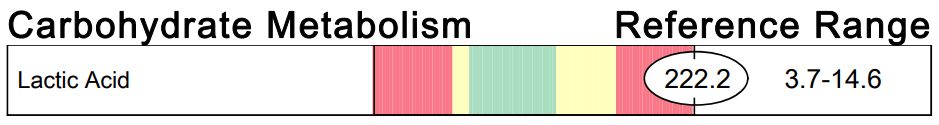
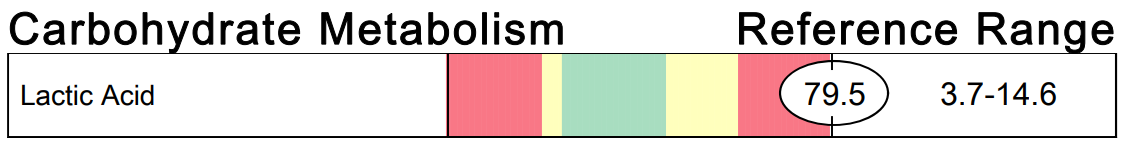
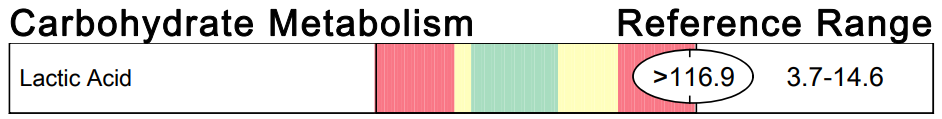
An elevation in lactic acid can indicate several things: thiamine deficiency, riboflavin deficiency, hypoxia from sleep apnea or other causes of impaired glucose metabolism. I most often see improvements in lactic acid levels after high dose benfotiamine has been started and the test is repeated. I've included three images of lactic acid results from my patients with DS below as examples, but have seen this many more times.
Aluminum
The main route of aluminum exposure in the body is through digestion as aluminum is the most abundant metal in the earth's crust. Aluminum present in soil eventually makes its way into the food and water we ingest. Fortunately, the lining of our digestive tract creates an effective barrier to the absorption of most consumed aluminum. Unfortunately, this barrier can be disrupted in states of ill-health and increased gastrointestinal permeability, aka leaky gut. Studies have shown that increased aluminum absorption through the GI tract occurs in those with AD.(Moore 2000) Citrate is another factor that can increase aluminum absorption.(Taylor 1998) I often recommend avoiding supplements like magnesium citrate to my patients for this reason.
A secondary source of aluminum that bypasses the gastrointestinal barrier is aluminum hydroxide that is the most common adjuvant used in vaccinations. Exposing the body to aluminum in this way completely bypasses the body's natural means of eliminating it. Aluminum, even in low levels, is a well-established neurotoxin. (Banks 1989, Joshi 1990, Krishnan 1988) As well, there is evidence for aluminum retention within the brain increasing the risk of neurotoxicity with multiple exposures. (Kumar 2014, Gherardi 2015) Dr. Exley and his team tested several commercially available aluminum based adjuvants, including Alhydrogel®, the most commonly used aluminum based adjuvant. This aluminum based adjuvant is in the form of aluminum oxyhydroxide. They revealed that this adjuvant "is most pre-disposed to migration away from the injection site..." to other areas of the body including the brain. (Exley 2016)
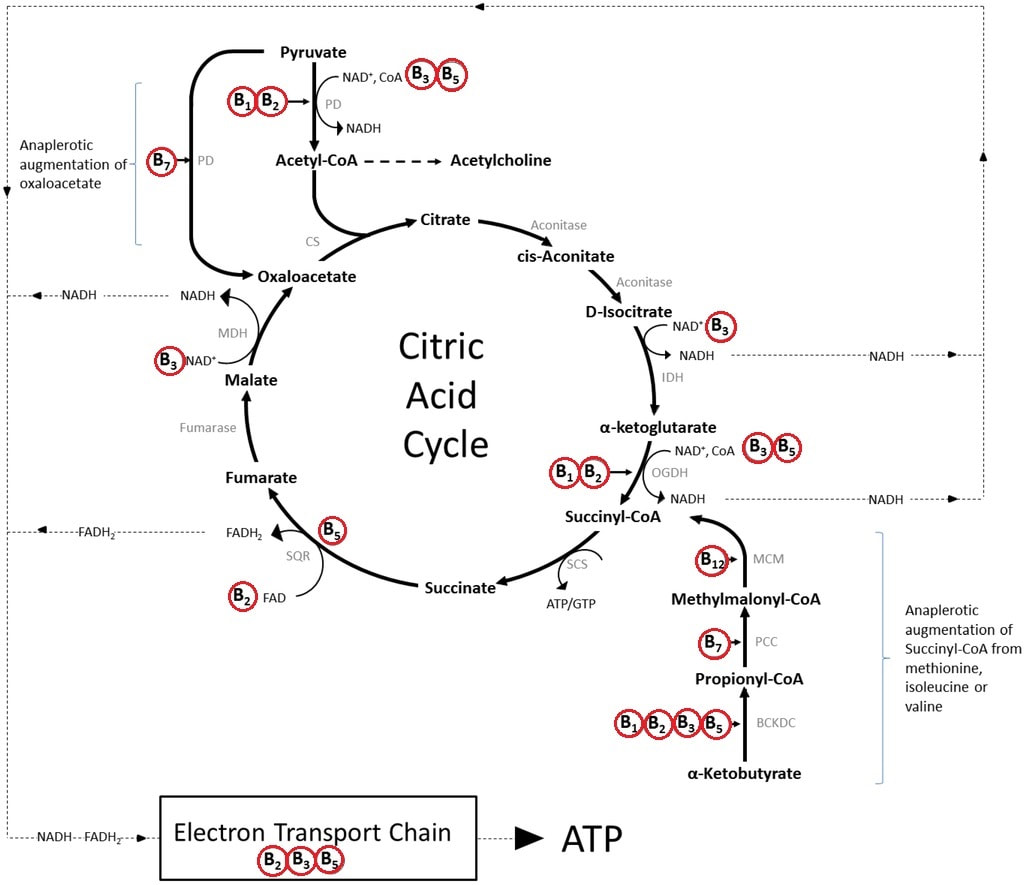
There is a growing body of evidence implicating mitochondria dysfuntion as the means by which aluminum causes neuronal damage. (Marchi 2004, Murakami 2004, Niu 2005) It has specifically been shown to interfere with isocitrate dehydrogenase (IDH) that is a NADPH dependent enzyme within the citric acid cycle (Image 5).(Murakami 2004) A decrease in this enzyme makes cells more sensitive to lipid peroxidation and oxidative mitochondria DNA damage. (Kim 2003, Lee 2002)
Aluminum can be a contributing factor to AD for those with DS. It's been shown that those with DS have an increase in gastrointestinal absorption of aluminum. (Moore 1997) It's likely due to the higher incidence and under-recognized rate of SIBO (small intestinal bacterial overgrowth) and gastrointestinal candida overgrowth. (Riordan 2002, Kumamoto 2001)
Mitochondria Dysfunction
The evidence pointing to mitochondria dysfunction in AD is strong and growing as well. I've pointed out several means above by which mitochondria function can be impacted. "Mitochondrial function is deregulated in AD and there is growing interest in understanding how altered mitochondrial function may be targeted to inhibit neurodegeneration." (Onyango 2016)
The most basic fuel that mitochondria need to make energy is oxygen and glucose. The process is similar in some ways to the burning of wood to create energy in the form of heat and light from a flame. Glucose in the wood is in the form of cellulose. Wood (glucose) also requires oxygen to burn. The same is true for our bodies. However, because the creation of energy within our bodies is tightly controlled by enzymes it's a bit more complicated than that. Those enzymes that control mitochondria energy production require B vitamins, particularly B1, B2, B3, B5, B6, B7, B9, B12...well, all of them. For those who are familiar with the citric acid cycle and how energy is generated from it, Image 5 shows how extensively the B vitamins are needed for it to operate. To learn more about mitochondria function you can read "Mitochondria - Why they're important and what they need to function".
Many studies exist supporting the presence of mitochondria dysfunction in those with DS. Coscun and Busciglio do a thorough job reviewing the role that mitochondria dysfunction has on the phhenotype of those with DS. (Busciglio 2012) In it they state, "Besides oxidative damage, mtDNA mutations and mitochondria dysfunction emerge as important modulators of DS phenotypes." Supporting mitochondria function in those with DS could greatly impact their risk of developing AD.
Ethical Dilemma
While ACI-24 may indeed create an immune response in the body that attacks amyloid plaque. Is it addressing the real underlying cause of the plaque? What are the consequences to the body if the underlying cause isn't addressed? Let's take thiamine deficiency for example. Thiamine deficiency in a mouse model has been shown to "greatly exacerbate plaque formation" (Gibson 2016) and you now know how thiamine can help prevent and possibly treat AD in humans. So, if we remove the plaque but don't address the thiamine deficiency will the brain and the rest of the body still struggle? It absolutely will. In addition, researchers from Cambridge, MA reviewed the possible protective role that amyloid plaque plays in protecting the brain in "Amyloid deposits - Protection against toxic protein species?". (Treusch 2009). Clearly, more information is needed about the nature of amyloid plaque before a drug or vaccine designed to remove it is developed.
Informed consent is an important and essential part of every ethical human study. Many parents hold guardianship over their adult children with DS and can sign consent for them to receive the experimental vaccine. As well, many adults with DS are perfectly able to understand the implications of, rate of and importance of preventing AD in DS when signing such a consent. However, are parents and those with DS getting all of the information about the yet undetermined cause of AD? Are they being shown or seeing research that supports alternatives to the amyloid plaque theory? Are they truly informed when they sign a consent? I fear not.
Research on human subjects must pass rigorous ethical standards. Guidelines for informed consent have been established by the Office for the Protection of Research Subjects. A full list of the basic elements for informed consent can be found in "Informed consent: Issues and challenges". (Nijhawan 2013). A key aspect of informed consent that should be highlighted here is "A disclosure of any appropriate alternative procedures or courses of treatment that might be advantageous to the subject". Based on what you've read here so far you can see that alternatives do exist. It's likely that subjects and their guardians or parents are not being told of the research supporting alternative means to prevent AD.
The DS population does hold a lot of information about the etiology of AD. However, it's not due to their genetics alone. The metabolic differences experienced in DS hold many clues as well. Researching the effects of addressing these metabolic differences would go a lot further and be much less costly than developing a vaccine that only addresses amyloid plaque.
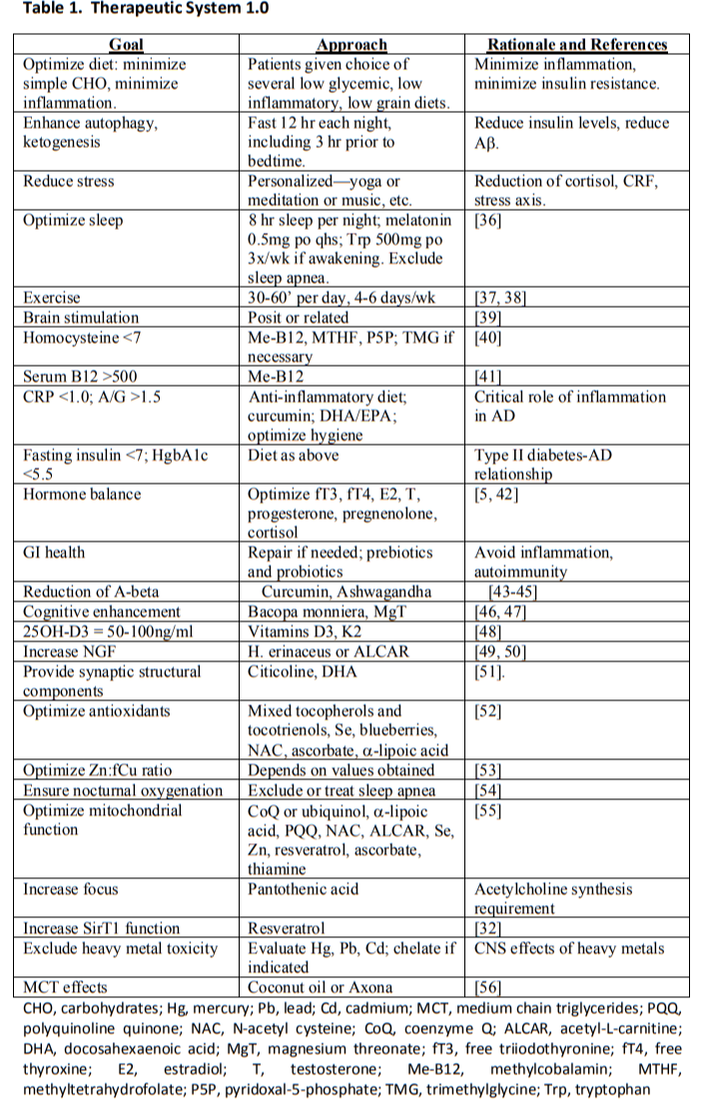
Optimal Treatment
Conclusion
I'll close by modifying an analogy made by Dr. Bredesen in his book that he calls "36 holes in the roof." The problem of neurodegeneration and dementia in AD is analogous to the problem of a house with many holes in the roof. Some holes are larger than others. Ideally, all holes would be fixed in order to keep the house dry. If a few small holes were left we might be able to manage and keep the house fairly dry inside. Let's imagine that the home owner is convinced that one of the larger holes is the only problem. He works diligently to repair only that hole while standing right outside his front door is a team of people willing to help repair the other holes. The home owner chooses to ignore this team of people and focus only on the one hole. This scenario would be frustrating to witness would it not?



 RSS Feed
RSS Feed