| I really miss teaching Cell Biology to college students. It gave me great satisfaction to teach them about the amazing machinery that exists within their bodies. My passion for this subject was evident in my lectures. I'm writing this blog post to help parents understand this subject that is so often mentioned online. I will explain here normal mitochondrial physiology then discuss mitochondrial dysfunction arising from vitamin deficiencies and biochemical disturbances that can interfere with their function. I will not be discussing genetic defects in mitochondrial DNA that impact how they function as this is a whole topic unto itself. |
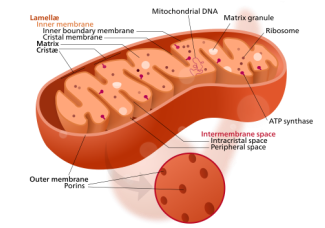
To say that mitochondria are important to human health is grossly understating their role in our survival. We literally would not be alive without them. They're fascinating organelles that convert our food into energy so that every other function of our body can occur. Basic mitochondrial function is typically taught based on how glucose is used to make energy, but proteins and fats are used to make energy as well.
To really break it down, this whole process is really all about moving electrons. Electrons are the energy of life. They're considered subatomic particles, but they have no matter or substance to them; they're made up of nothing but energy. Every chemical process that occurs in your body happens because electrons and the energy from them are transferred to enable these processes to occur.
The terms "reduction" and "oxidation" should be explained here as they describe how electrons are transferred. Reduction occurs when a compound gains an electron, which gives the compound more negative charge, basically "reducing" it's charge. Oxidation occurs when a compound loses an electron. This term is used for this process because oxygen is the most common electron "thief" within the body.
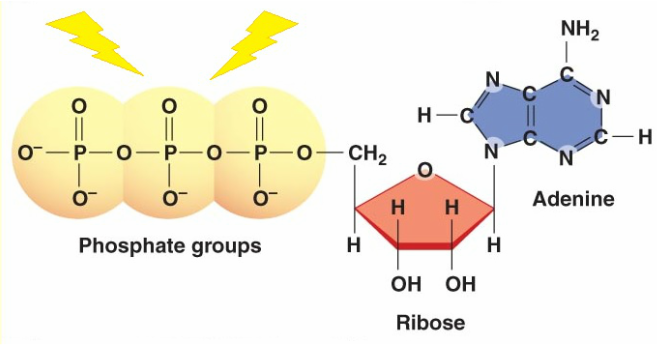
Electrons are typically carried and transferred from a high energy compound called ATP (image 1). ATP carries energy between its highly energized phosphate groups (yellow). You can see in the image that they are all negatively charged. They really don't want to be next to each other (recall that positive and negative charges attract one another and negative charges typically repel each other). Their negative charges come from an extra electron that they are carrying. It's these electrons that are transferred in order to give energy to millions of chemical processes within our body. When ATP releases one of these phosphate groups to a reaction it causes that reaction to move forward.
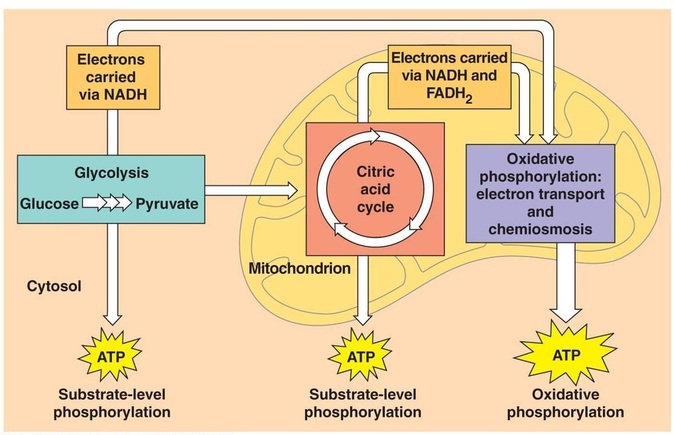
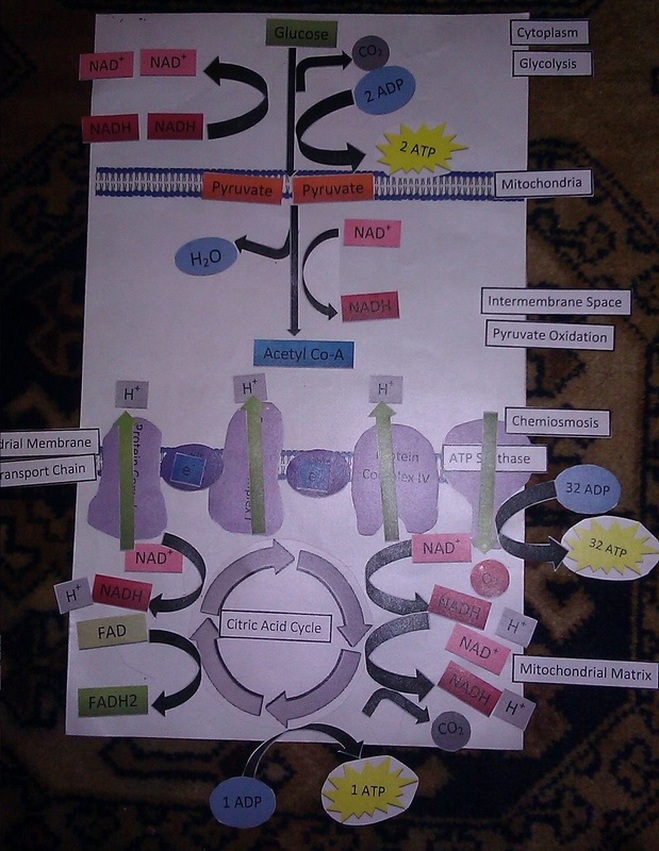
- Glycolysis
- Pyruvate Oxidation
- Citric Acid Cycle (Krebs Cycle or Tricarboxylic Acid Cycle - TCA)
- Electron Transport Chain (Oxidative Phosphorylation)
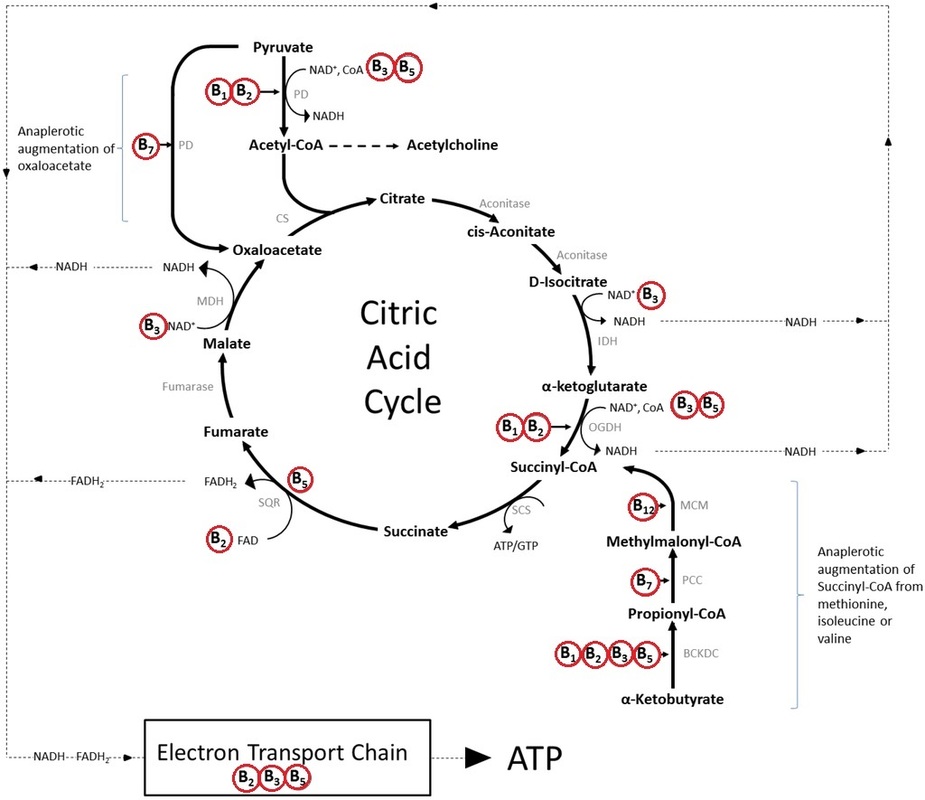
I will focus on the steps that occur within the mitochondria only. Those are the Citric Acid Cycle and the Electron Transport Chain. These last two steps can only occur in the presence of sufficient amounts of oxygen. When oxygen levels are low, like in sleep apnea or during times of intense exercise when oxygen demand from muscles exceeds available oxygen, pyruvate cannot be shuttled into the mitochondria. Lactic acid fermentation is used instead which is much less efficient and generates only two ATP molecules.
The following video reviews the basic steps in the Citric Acid Cycle. Keep in mind, this is a basic representation and there are many other factors that are involved. You should also know that ubiquinone is CoQ10.
If you're craving even more information on this topic, this chapter of the The Cell by Alberts B, Johnson A, Lewis J, et al. outlines these processes in much greater detail: The Mitochondrion.
The areas of highest mitochondrial activity, based on the rate of ubiquinone reduction and oxidation, are the heart, kidney and liver (1). As well, because the brain is the most metabolically active organ in the body it is vulnerable to disruptions in mitochondrial function.
Several researchers have reported a connection between mitochondrial dysfunction and autism (2,3,4). In addition, mitochondrial dysfunction in Down syndrome has been well-established (5). Many biomedical clinicians have already come to accept that mitochondrial dysfunction is something to look for and treat in children with autism and other special needs. As well, many parents are seeing notable improvements in their children's health and development when mitochondria dysfunction is detected and addressed.
Because so many organs and processes of the body are dependent on ATP and the mitochondria that makes it, symptoms can be vague and impact many organ systems. These symptoms include:
- Low muscle tone
- Difficulty swallowing
- Failure to thrive
- Learning disability
- Fatigue
- Delayed gut motility
- Heat/cold intolerance
- Migraines
- Lactic acidosis
- Liver disease
- Immune system problems
- Heart problems
- Kidney problems
- Neurological problems
- Autonomic dysfunction
You can see how easily a doctor might dismiss these symptoms as Chronic Fatigue Syndrome, Irritable Bowel Syndrome or no diagnosis is made and "there's nothing that can be done". Many times pharmaceutical drugs will be used that mask these symptoms yet never really help the patient nor address the root cause of the patient's problem.
All of the above steps don't just magically happen. Each of the steps requires an enzyme to make it happen and those enzymes have cofactors that are required in order for them to work. In addition, nutrients don't just automatically cross into the mitochondria; some are shuttled in with carriers.
Compounds they require to function properly:
- CoQ10
- B Vitamins
- L-Carnitine
- D-ribose
- Iron
- Alpha lipoic acid (6)
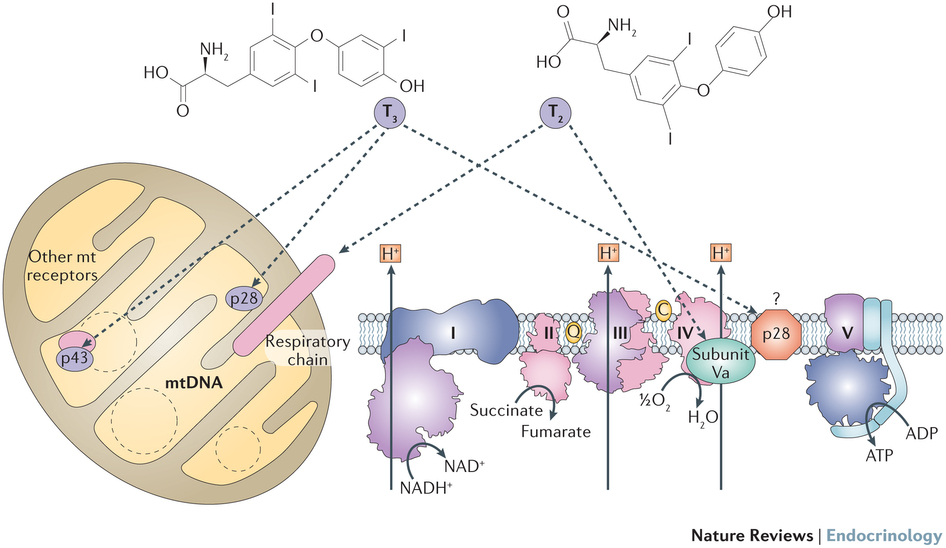
- Thyroid hormone (T3 and T2)
- Ubiquinone - fully oxidized, missing both electrons it's capable of carrying
- Semiquinone - missing one electron
- Ubiquinol - fully reduced, carrying both electrons it can can carry
Ubiquinone is typically used as a supplement when mitochondria support is the goal. Ubiquininol can be used as an antioxidant because it carries two electrons that can be used to limit the damage caused by reactive oxygen species (ROS). ROS create damage because they have an unpaired electron that is seeking to be matched with another electron. This extra electron can be gained from lipids within the body or from DNA, which damages these structures. Ultimately antioxidants are electron donors and ubiquinol is one of many electron donors that serve as antioxidants. The role of CoQ10 within the mitochondria is as an elecron carrier, so ubiquinone is best. CoQ10 has been shown to lower levels of oxidized purines, which are the damaged pieces of DNA that occur as a result of oxidative stress, in cells of those with Down syndrome (7).
B vitamins are needed as enzyme cofactors for each step of the TCA and within the electron transport chain (image 4). These B vitamins can quickly become depleted in a diet that contains processed grains because those grains provide glucose but are stripped of the bran and germ that contain B vitamins to help our bodies get energy from the glucose. Deficiencies in B vitamins are also very common in those who have an imbalance in their gut flora like small intestinal bacterial overgrowth (SIBO) or candida overgrowth (8).
Lastly, carnitine deficiency has been shown to cause delayed gut motility leading to vomitting after meals, oral drooling, delayed gastric emptying and constipation (13). This makes sense given how much muscle function is impacted by mitochondria function and optimal gut motility is a consequence of healthy muscle function.
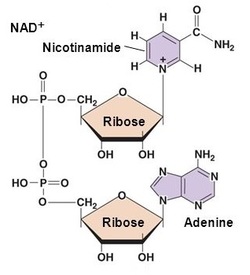
| Ribose is a five-carbon sugar that is made in the body from glucose. It's a component of ATP and NADH/NAD+. Image 1 (above) shows ribose as a part of ATP. You can see in image 5 how NAD+ requires two ribose molecules. A recent mouse study found that ribose increased gut motility and improved their resistance to weight gain through improved energy homeostasis (14). Supplementing with D-ribose has also been shown to be helpful for chronic fatigue and fibromyalgia patients through it's ability to increase cellular energy (15). Moreover, ribose may provide protection to cells during states of elevated oxidative stress, which children with autism and Down syndrome experience (16). Because muscle tone and function is so dependent on mitochondrial function and ATP many studies exist supporting ribose's role in muscle energetics (17). |
Alpha lipoic acid (ALA) is a fatty acid that is synthesized within mitochondria and acts as a very potent antioxidant. It can also be obtained in the diet in the form of lipoyllysine and is highest in animal tissue (kidney, heart, liver) and green plants like spinach and broccoli (18). In addition to being an antioxidant ALA is also required as a cofactor for one of the enzyme complexes that makes up pyruvate dehydrogenase. This enzyme complex converts pyruvate (made from glucose) to acetyl-CoA that is the entrance point for the TCA. It's thought that ALA deficiency doesn't exist as the body typically makes what it needs. However, supplementing with ALA has been shown to support brain health, cardiovascular health, heavy metal chelation, insulin function and inflammation (19, 20). It's repeatedly been shown to work well when supplemented together with acetyl l-carnitine (21,22, 23, 24).
- Plasma free carnitine and acylcarnitine
- Urine organic acid test (TCA cycle intermediates, lactic acid, pyruvic acid, ketone and fatty acid oxidation, 3-methylglutaric, 3-hydroxyglutaric, 3-methylglutaconic)
- Plasma amino acids, alanine:lysine ratio or elevated alanine (27)
Not all doctors will order these tests, nor will they know how to interpret them. It's important to work with a doctor who has training or is educated to understand these tests. Interpreting these labs is both simple yet complicated. For example, if carnitine levels are low supplementation is warranted. Other markers that indicate a need for carnitine are urinary fatty acids, adipic and suberic acid. When they are elevated in the urine it indicates that they are not being shuttled into mitochondria and not being used, hence the need for carnitine. Doses recommended are in the range of 20-100 mg/kg/day for children (28). Elevated urinary pyruvic acid can indicate a need for alpha lipoic acid as well as B1, B2 and B3. Elevated intermediates of the TCA in the urine can indicate a need for cofactors of the enzyme needed to convert that intermediate to the next step of the TCA, typically these are B vitamins. This information is greatly simplified and assessment of what each patient needs to support their individual mitochondrial needs requires an evaluation from a trained physician.
Mitocondrial dysfuntion is currently not recognized by conventional medical physicians who often choose to prescribe pharmaceuticals for symptoms in lieu of addressing the root cause of disease. Fortunately physicians who are trained in mitochdondrial function exist and include Functional Medicine practitioners, Naturopathic physicians, Biomedical doctors and MAPS doctors.
- Aberg F., Appelkvist E.L., Dallner G., Ernster L. Distribution and redox state of ubiquinones in rat and human tissues. Arch. Biochem. Biophys. 1992;295:230–234.
- Palmieri L, Persico AM. Mitochondrial dysfunction in autism spectrum disorders: cause or effect?Biochim Biophys Acta. 2010;1797(6–7):1130–7.
- Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry 2012; 17: 290–314.
- Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry. 2012;17(3):290–314.
- Helguera P, Seiglie J, Rodriguez J, Hanna M, Helguera G, Busciglio J. Adaptive Downregulation of Mitochondrial Function in Down Syndrome. Cell metabolism. 2013;17(1):132-140.
- Nicolson GL. Mitochondrial dysfunction and chronic disease: treatment with natural supplements. Altern Ther Health Med. 2013
- Tiano L., Busciglio J. Mitochondrial dysfunction and Down’s syndrome: is there a role for coenzyme Q10? BioFactors. 2011;37(5):386–392.
- Dibaise, JK. Nutritional Consequences of Small Intestinal Bacterial Overgrowth. Nutrition Issues in Gastroeneterology. December 2008.
- Kumaran S, Subathra M, Balu M, Panneerselvam C. Supplementation of L-carnitine improves mitochondrial enzymes in heart and skeletal muscle of aged rats. Experimental Aging Research.2005;31(1):55–67.
- Seven M, Cengiz M, Tüzgen S, Iscan MY. Plasma carnitine levels in children with Down syndrome.Am J Hum Biol. 2001 Nov–Dec;13(6):721–5.
- Picard M, McEwen BS. Mitochondria impact brain function and cognition.Proceedings of the National Academy of Sciences of the United States of America. 2014;111(1):7-8.
- Montgomery S., Thal L., Amrein R. Meta-analysis of double blind randomized controlled clinical trials of acetyl-L-carnitine versus placebo in the treatment of mild cognitive impairment and mild Alzheimer’s disease. Int. Clin. Psychopharmacol. 2003;18:61–71.
- Weaver LT, Rosenthal SR, Gladstone W, Winter HS. Carnitine deficiency: a possible cause of gastrointestinal dysmotility. Acta Paediatr. 1992 Jan;81(1):79-81.
- Liu Y, Li T-RR, Xu C, Xu T. Ribose Accelerates Gut Motility and Suppresses Mouse Body Weight Gaining. International Journal of Biological Sciences. 2016;12(6):701-709.
- Teitelbaum J. E., Johnson C., St. Cyr J. The use of D-ribose in chronic fatigue syndrome and fibromyalgia: a pilot study. Journal of Alternative and Complementary Medicine. 2006;12(9):857–862.
- Addis P, Shecterle LM, Alexander J. Cellular protection during oxidative stress: A potential role for d-ribose and antioxidants. J Diet Suppl. 2012, 9 (3).178-82.
- Dodd SL, Johnson CA, Fernholz K, St Cyr JA. The role of ribose in human skeletal muscle metabolism.Medical hypotheses. 2004;62:819–24.
- Lodge JK, Youn HD, Handelman GJ, et al. Natural sources of lipoic acid: determination of lipoyllysine released from protease-digested tissues by high performance liquid chromatography incorporating electrochemical detection. J Appl Nutr. 1997;49(1 & 2):3-11.
- Shay KP, Moreau RF, Smith EJ, Smith AR, Hagen TM. Alpha-lipoic acid as a dietary supplement: Molecular mechanisms and therapeutic potential.Biochimica et biophysica acta. 2009;1790(10):1149-1160.
- Gomes MB, Negrato CA. Alpha-lipoic acid as a pleiotropic compound with potential therapeutic use in diabetes and other chronic diseases. Diabetology & Metabolic Syndrome. 2014;6:80.
- McMackin CJ, Widlansky ME, Hamburg NM, et al. Effect of Combined Treatment with Alpha Lipoic Acid and Acetyl-L-Carnitine on Vascular Function and Blood Pressure in Coronary Artery Disease Patients. Journal of clinical hypertension (Greenwich, Conn). 2007;9(4):249-255.
- Zhang H, Jia H, Liu J, et al. Combined R-α–lipoic acid and acetyl-L-carnitine exerts efficient preventative effects in a cellular model of Parkinson’s disease.Journal of Cellular and Molecular Medicine. 2010;14(1-2):215-225.
- Kumaran S, Savitha S, Anusuya Devi M, Panneerselvam C. L-carnitine and DL-α-lipoic acid reverse the age-related deficit in glutathione redox state in skeletal muscle and heart tissues. Mechanisms of Ageing and Development. 2004;125(7):507–512.
- Soczynska JK, Kennedy SH, Chow CS, Woldeyohannes HO, Konarski JZ, McIntyre RS. Acetyl-L-carnitine and alpha-lipoic acid: possible neurotherapeutic agents for mood disorders? Expert Opin Investig Drugs. 2008;17(6):827–843.
- Kvetny J, Wilms L, Pedersen PL, Larsen J. Subclinical hypothyroidism affects mitochondrial function.Hormone and Metabolic Research. 2010;42(5):324–327.
- Wrutniak-Cabello C., Casas F., Cabello G. Thyroid hormone action in mitochondria. J. Mol. Endocrinol.2001;26:67–77.
- Haas RH, Parikh S, Falk MJ, et al. The In-Depth Evaluation of Suspected Mitochondrial Disease: The Mitochondrial Medicine Society’s Committee on Diagnosis. Molecular genetics and metabolism. 2008;94(1):16-37.
- Parikh S, Saneto R, Falk MJ, et al. A Modern Approach to the Treatment of Mitochondrial Disease. Current treatment options in neurology. 2009;11(6):414-430.


 RSS Feed
RSS Feed